Dental and Gum Disorders (Periodontal Disease) of the Cavalier King Charles Spaniel
-
 Tooth Anatomy
Tooth Anatomy - What Is Peridontal Disease
- Cavalier's Unique Form of PD
- Symptoms
- Diagnosis
- Prevention
- Related Disorders
- Treatment
- Genetics
- Breeders' Responsibilities
- Other Dental Disorders
- What You Can Do
- Research News
- Related Links
- Veterinary Resources
Cavalier King Charles spaniels are more susceptible to a dental and gum and bone-loss disorder called periodontal disease (PD) than most any other dog breeds. See What is Periodontal Disease, below. While PD is the most commonly diagnosed disease in dogs, the CKCS suffers from an earlier-onset version in which the the gums recede and the tooth roots become exposed as early as two years of age.
In an April 2015 article, a team of UK veterinary researchers reviewed the primary-care medical records of 1,875 cavalier King Charles spaniels from July 2007 to July 2013. They categorized the most common specific disorders recorded by the examining veterinary clinicans, as follows: First were heart murmurs, followed by dental disease, including periodontal disorders. Dental disorders were included only when severe enough to result in a veterinary recommendation for medical or surgical intervention.
In an August 2021 review of the prevalence of PD in dogs treated at UK veterinary clinics, cavaliers ranked fourth (behind greyhounds, King Charles spaniels, and toy poodles), and in a July 2021 article, CKCSs were found to have the highest probability of PD in the medium-small size category treated at a nationwide chain of USA clinics.
In a poster presented at the March 2024 BSAVA 2024 conference, UK researchers found that among 177 cavaliers surrendered to a cavalier rescue group, the second most common health condition (after painful Chiari-like malformation) was dental disease requiring extractions, numbering 121 cavaliers (68.45%). The data was collected from a combination of questionnaires, health checklists, veterinary medical histories, and veterinary examinations following surrender.
Read our section below -- Cavalier's Unique Form of PD -- to find out why CKCSs may be so susceptible to an early-onset version of periodontal disease.
RETURN TO TOP
Tooth Anatomy
 Puppies
are born toothless, and then they develop 28 puppy teeth, also called "milk teeth" or
"deciduous teeth", after they reach about three weeks of age. At about
the age of three to five months, their 42 permanent teeth begin to appear,
replacing the puppy teeth. This process usually is complete by the
seventh month. If the baby teeth do not fall out (exfoliate) before the
permanent teeth begin to appear, the condition is called
persistent deciduous teeth,
discussed below.
Puppies
are born toothless, and then they develop 28 puppy teeth, also called "milk teeth" or
"deciduous teeth", after they reach about three weeks of age. At about
the age of three to five months, their 42 permanent teeth begin to appear,
replacing the puppy teeth. This process usually is complete by the
seventh month. If the baby teeth do not fall out (exfoliate) before the
permanent teeth begin to appear, the condition is called
persistent deciduous teeth,
discussed below.
From the front to the rear, the permanent teeth consist of 12 incisors, 4 canines, 16 premolars, and 10 molars. (See diagram below.)
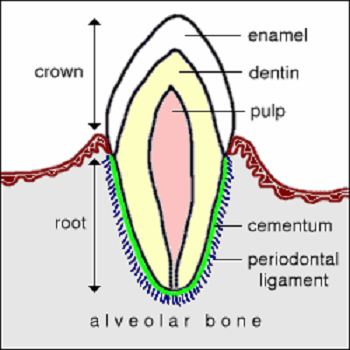
As this diagram (right, from ColoSate Univ.) shows, a typical tooth consists of the visible portion above the gumline, called the "crown", and the portion beneath the gumline, called the "root". The crown consists of the enamel exterior, within which is dentin and pulp.
The root is surrounded by the "periodontal ligament" and a thin coating called "cementum" and then the jaw bone, called "alveolar bone". The root includes nerves and blood vessels which are connected at the bottom, called the "root end opening".
The gums are called the "gingiva". They surround the teeth and cover the alveolar bone. Healthy gums normally are pink, unless the breed has pigmented gums.
The gums (gingiva), periodontal ligament, cementum, and alveolar bone make up the periodontium.
RETURN TO TOP
What is Periodontal Disease
"Periodontal" means "around or near the teeth", referring to the tissues which hold the teeth in place in the jaw. While periodontal disease (PD) affects the teeth, it actually is an inflammatory disease of the periodontium -- the gums (gingiva), periodontal ligament, cementum (mineralized tissues lining the root), and/or alveolar bone. (See diagram above.) PD is defined as periodontal pockets greater than 3 mm in depth. A pocket is a gap in the gums surrounding the tooth. The presence of plaque, and even gingivitis, technically are not PD.
 Plaque
Plaque
PD usually is a late stage of a series of infectious disorders which begin when bacteria, such as Porphyromonas gulae, which enter the dog's mouth, adhere to its teeth, both above and below the gumline, and to the gums themselves in the form of a biofilm called plaque. Plaque consists of saliva, food particles, and hundreds of bacterial microbes. Extracellular polysaccharides (EPS) are sugars from some foods which become the backbone of the biofilm and ensure that bacteria are able to attach to the plaque. The accumulation of plaque is the cause of PD.
Plaque can attach to the teeth and gums within twenty-four hours if not subject to daily cleaning. Plaque on the tooth surface above the gumline is called supragingival plaque. Supragingival plaque can be treated and then reversed in most cases by daily dental care. Within three days, undisturbed plaque becomes calcified by minerals in the dog's saliva, becoming calculus or tartar (See photo of brownish calculus on a dog's tooth, at right.) Calculus forms from plaque when calcium salts in the saliva mineralize the plaque. The calculus (or tartar) encases the bacteria and permits it to spread unimpeded.
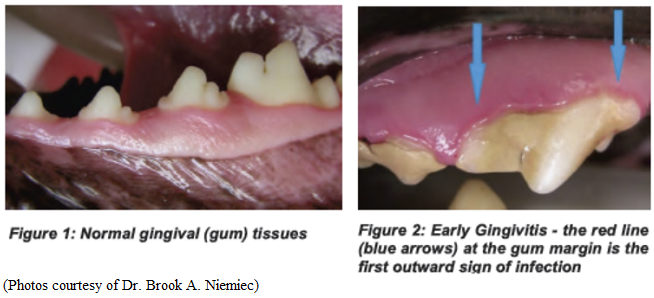
Gingivitis
If the biofilm plaque is not removed by daily cleaning, the bacteria
adhere to the gums (the gingiva)
 and cause inflammation
which is called gingivitis. (See photo at right.)
This process can occur in as early as two weeks.
and cause inflammation
which is called gingivitis. (See photo at right.)
This process can occur in as early as two weeks.
If left untreated, the plaque will advance by extending under the gums between the teeth and underlying alveolar bone, a stage called subgingival plaque. The presence of the darkened tartar on the visible crowns serve as an early warning that the dog has a potential PD problem which needs professional veterinary attention. Therefore, the plaque must be removed from both above and below the gumline to defeat the progression of the gingivitis to becoming PD.
While the hardened tartar is visible on the crown of the teeth as a stained coating, that does not cause PD. It is the plaque beneath the gumline -- the subgingival plaque -- which causes gingivitis, the precursor of PD.
Periodontal Pocket
The inflammed gums will start to recede from the tooth, creating a gap called a periodontal pocket. These pockets create hiding places for the plaque and tartar, and eventually the pockets deepen down along the roots of the teeth. As long as those pockets are no deeper than 3 mm, gingivitis can be reversed by a thorough professional cleaning -- scaling of each tooth -- and PD can be avoided.
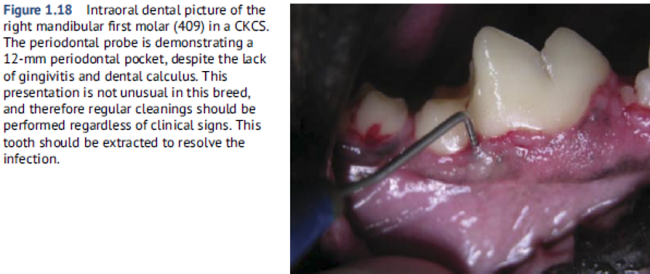
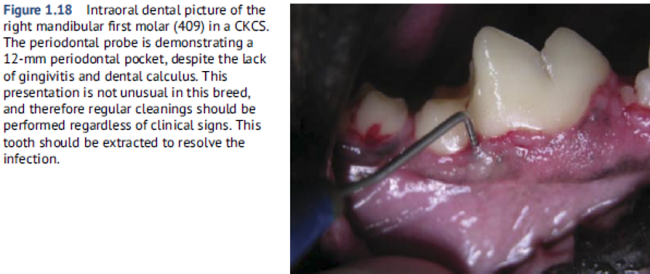 In
Figure 1.18 at right from his book,
Breed Predispositions to Dental
and Oral Disease in Dogs, Dr. Brook Niemiec
displays such a periodontal pocket at the right first molar of a
cavalier. In this case, the dog does not have evidence of gingivitis or
calculus. He points out that the lack of those signs is not unusual for
CKCSs, which warrants the need for regular cleanings despite the lack of
any clinical signs.
In
Figure 1.18 at right from his book,
Breed Predispositions to Dental
and Oral Disease in Dogs, Dr. Brook Niemiec
displays such a periodontal pocket at the right first molar of a
cavalier. In this case, the dog does not have evidence of gingivitis or
calculus. He points out that the lack of those signs is not unusual for
CKCSs, which warrants the need for regular cleanings despite the lack of
any clinical signs.
Periodontitis
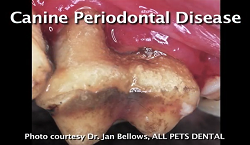 Periodontitis
is an inflammation of the periodontal ligaments benealth the gums and of the alveolar
bone, resulting in their destruction and leading to more recession of the
gums and the formation of periodontal pockets deeper than 6 mm, and then bone loss. this process usually takes two to five years
to develop in most large breeds. (See
photo at right.)
Periodontitis
is an inflammation of the periodontal ligaments benealth the gums and of the alveolar
bone, resulting in their destruction and leading to more recession of the
gums and the formation of periodontal pockets deeper than 6 mm, and then bone loss. this process usually takes two to five years
to develop in most large breeds. (See
photo at right.)
Furcation
The final stage of PD, also called furcation disease, is recession of the gums and bone to the point that the area between the roots become exposed, leading to tooth loss and potentially a host of related systemic disorders, due to the bacteria's access to the blood stream.
RETURN TO TOP
Cavalier's Unique Form of PD
 Periodontal disease is the most commonly diagnosed disease in
all dogs, and it is known to develop earlier in small and toy breeds
than in larger ones. In the cavalier, PD is second only to mitral valve
disease, and yet, PD is more prevalent in the CKCS than in any other
breed.
Periodontal disease is the most commonly diagnosed disease in
all dogs, and it is known to develop earlier in small and toy breeds
than in larger ones. In the cavalier, PD is second only to mitral valve
disease, and yet, PD is more prevalent in the CKCS than in any other
breed.
As noted above, the usual progression of PD starts with the biofilm of plaque, then the hardening of the plaque into tartar above the gums and into subgingival plaque beneath, and then gingivitis, and then periodontitis. Each phase typically takes time in the mouth of the average dog. Plaque attaches to the teeth in 24 hours. Plaque turns to tartar (calculus) in three days. Gingivitis can develop below the gums in two weeks. Periodontitis may take two to five years. However, the cavalier King Charles spaniel breed has been found to suffer from an earlier-onset version in which PD develops much more rapidly and by-passes the usual time-line of progression. Cavaliers reportedly can develop severe periodontitis with minimal tartar build-up or visible gum infection -- the usual early-warning signs of PD. (See Figure 1.18, below.)
The reasons for the cavaliers' early-onset version of PD have not been proven, but the breed's evolutionary history is suspected. All dogs, regardless of how big or small they are or how long or short their muzzles are, have the same number of adult teeth -- 42. Most brachycephalic breeds, with their shorter muzzles, tend to suffer from tooth crowding, having their rows of teeth somewhat jumbled, with teeth overlapping each other as all 42 of them try to fit into a much shorter mouth than those of their earlier ancestors with much longer snouts. The cavalier is an even more convoluted example of this evolution, because in the late 1920s the breed developed from the even-shorter muzzled King Charles spaniel (English toy spaniel).
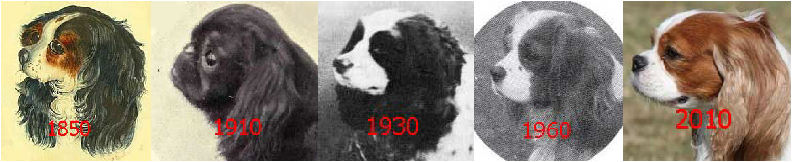
Most of the earlier versions of the King Charles spaniel (KCS), up to
the late 1800s, had relatively long muzzle lengths. (See the 1850
version, above.) Then, beginning in
the 1890s through the 1920s, the breed standard called for their snouts
to be bred much shorter. By 1910, champion King Charles spaniels had
snouts no longer than those of today's pugs and French bulldogs.
(See the 1910 champion KCS, above.) Breeders still produced
longer-muzzled KCS puppies, but they did not intentionally breed them.
In 1926, an American dog fancier campaigned to bring back the
longer-muzzled "old type" King Charles spaniel, and by the early 1930s,
the new breed, the "cavalier" King Charles spaniel, came into being
after breeders started selecting their longer-snouted offspring for
breeding and then competing with them at Crufts and other UK
conformation shows as a breed different from the KCS. (See the
series of photos above to follow the transition to the first of the
cavaliers in the 1930 photo, followed
 by
more recent examples.)
by
more recent examples.)
A consequence of this evolution was first to create very short-muzzled dogs with necessarily extremely jumbled sets of teeth, and then produce from those dogs a longer-muzzled version which became the cavalier. The compressed set of teeth in the KCS did not conveniently re-arrange themselves into an orderly, straightened line up in the longer mouths of the CKCS. So, the typical cavalier's mouth has been the result of an accordion-like compression and then enlongation of teeth, resulting in mass confusion. (See the photo at right of a CKCS mouth.)
In a December 2022 article, veterinary dental specialists found that cavaliers are among the most commonly affected breeds of abnormal alignment and positioning of their upper and lower sets of teeth. In that case, the researchers examined the records of 198 dogs presented to a California veterinary dental clinic with misalignment (malocclusion) of either their baby teeth (deciduous) or permanent teeth. There are two types of malocclusions: (1) skeletal, which means that an abnormal jaw length results in a misalignment of the teeth, and (2) dental, which occurs when one ore more teeth are out of normal alignment, also called malpositioned teeth. In this California study, which spanned from 2015 to 2018, the cavalier, along with the poodle and Labrador retriever, comprised 50% of the dogs with deciduous (baby teeth) malocclusions. The five most commonly affected breeds with permanent malocclusions were the cavalier, along with poodles, Labrador retrievers, chihuahuas, and pit bull terriers. See also this December 2022 article.
RETURN TO TOP
Symptoms
Normal features of the dog's mouth are clean-looking teeth and pink gums (gingival tissues), without any staining of the teeth or redness or signs of inflammation in the gums. (See Figure 1 below.) In the early stage of gingivitis, the teeth will look stained by being partially coated with a somewhat dirty-looking calculus (tartar), and areas of the gums, particularly where directly attached to the teeth, will be puffy, redish, and appear inflammed. (See Figure 2 below.)
Bad breath (halitosis) can be a sign of tooth decay. But it also may be a sign of other disorders, including chronic kidney disease (CKD), diabetes, megaesophagus, and respiratory tract infections.
In his 2021 book, Breed Predispositions to Dental and Oral Disease in Dogs, Dr. Brook Niemiec observed that:
"Cavalier King Charles Spaniels (CKCS) ... are well known for significant periodontal disease. CKCS suffer from early onset periodontal disease, especially in the maxillary premolars (as they are similar to other brachycephalic breeds). There is quite often furcation exposure of these teeth as early as two years of age. Interestingly, it is quite common for them to have advanced periodontal loss with minimal calculus and gingivitis."
As the PD progresses, the inflammation will have spread and intensified. The discolored tartar will be more extensive. The gums will bleed or develop ulcers, and they will appear to bulge and to have receded. Eventually the teeth roots will become exposed. The dog's breath will be consistently bad (halitosis). Some of the teeth may become loose. White pus may discharge from the periodontal pockets.
The level of inflammation is the surest sign that professional care is needed.
RETURN TO TOP
Diagnosis
 Diagnosis is primarily a visual inspection of the teeth and gums. If
the dog is under anesthesia, the veterinarian will use a stainless steel
periodontal probe to poke
into the pockets to determine their depth and condition. X-rays of the
teeth and roots and bone will be necessary for a thorough analysis of
the extent of the condition of the PD.
Diagnosis is primarily a visual inspection of the teeth and gums. If
the dog is under anesthesia, the veterinarian will use a stainless steel
periodontal probe to poke
into the pockets to determine their depth and condition. X-rays of the
teeth and roots and bone will be necessary for a thorough analysis of
the extent of the condition of the PD.
Diagnosis beneath the gumline customarily is performed along with a thorough cleaning, while the dog is under anesthesia. See the Periodic Cleaning Procedures described below.
While periodic teeth scaling and polishing procedures (limited to above the gum-line) are not advised for the treatment of PD, a July 2021 study found that the longer time period since a scale-and-polish treatment increased the odds of PD being diagnosed and also more severe PD being found.
RETURN TO TOP
Prevention
Apart from breed-specific causes of the onset of tooth and gum
disease, studies have attributed causes to
 include
feeding dry dog foods and the lack of daily brushing of the dog's teeth.
In this
February 2024 article, for example, the author reported finding "a trend among dogs being fed dry foods
to develop periodontal disease."
include
feeding dry dog foods and the lack of daily brushing of the dog's teeth.
In this
February 2024 article, for example, the author reported finding "a trend among dogs being fed dry foods
to develop periodontal disease."
She also stated that "Regular dental brushing has been found to support significant treatment in patients who are still in the early stages of the disease, even while differences in the antibiotics used in medical treatment do not yield substantial differences in outcomes."
In a July 2025 article, 4,771 Finnish dogs' medical records were reviewed to determine early life factors contributing to reports of dental calculus (DC) and its risks and protective factors. They reported:
"Our research indicated that dogs fed a non-processed meat-based diet during the weaning period, puppyhood, and adolescence, which corresponds to the age range of 1 month to 1 or 1.5 years, were associated with a significantly lower risk of developing DC [dental calculus] later in life. Conversely, dogs consumed an ultra-processed carbohydrate-based diet during the same periods [weaning, puppyhood, and adolescence, respectively] was associated with a significantly higher risk."
To get back to dry dog foods (kibble): They do not clean dogs' teeth in any way, because dogs do not chew the kibble pieces. They swallow them whole.
RETURN TO TOP
Related Disorders
Inflammation and redness in the gums, due to gingivitis, are indications that blood capillaries are leaking, allowing the plaque bacteria access to the bloodstream. Once in the bloodstream, the bacteria travel to the vital organs -- the heart, lungs, kidneys, liver, and brain.
Localized Disorders
See Dr. Brook Niemiec's YouTube video, begining at 5:32 minutes, for a full review of these localized related disorders:
 • Oronasal fistula: As the PD progresses and the
gums, roots, and bone erode, a fistula (vacant gap) may develop into the
nasal cavity between
the the upper jaw and the nasal passage. This is called an oronasal
fistula (ONF). Infected ONFs must be surgically repaired, usually by
extracting the adjoining tooth and suturing a flap of tissue in the
mouth.
• Oronasal fistula: As the PD progresses and the
gums, roots, and bone erode, a fistula (vacant gap) may develop into the
nasal cavity between
the the upper jaw and the nasal passage. This is called an oronasal
fistula (ONF). Infected ONFs must be surgically repaired, usually by
extracting the adjoining tooth and suturing a flap of tissue in the
mouth.
• Fracture of the mandible: As the bone in affected areas of the lower jaw become weakened, the jaw may become so fragile that a slight trauma or even a tooth extraction could cause a fracture. Pre-surgical x-rays must be taken to locate the eroded bone and its remaining dimensions. Surgical options include inserting pins or wires or plates. Healing of this procedure can be quite difficult, and the usual prognosis is "guarded".
• Chronic ulcerative paradental stomatitis (CUPS): CUPS are extremely painful, inflammed sores and ulcers on the soft tissues which come in contact with the teeth (paradental areas). The are believed to be an allergic response to bacterial plaque on the teeth. See our webpage, Chronic Ulcerative Paradental Stomatitis (CUPS) and the Cavalier King Charles Spaniel.
• Eosinophilic stomatitis (eosinophilic granuloma): Cavaliers are predisposed to some eosinophilic syndromes, especially eosinophilic stomatitis, an autoimmune disorder which is an inflammation of the mucous lining of any parts of the mouth, such as the tongue, palate, and gums. It usually appears as ulcers and lesions on the surfaces within the mouth. See our webpage, Eosinophilic Stomatitis and the Cavalier King Charles Spaniel.
• Blindness: PD inflammation and infection close to an eye cavity (orbit) may jeapardize the optic tissues and lead to blindness.
• Osteomyelitis: Inflammation due to PD of bone or bone marrow may lead to infected, and even dead, bone tissue. This is called osteomyelitis, and the affected bone must be removed surgically.
• Oral cancer: Chronic inflammation due to PD may result in cancer in the mouth. See our webpage, Cancer and the Cavalier King Charles Spaniel.
• Meningoencephalitis: Meningoencephalitis is inflammation of the brain and its protective membranes, usually caused by a bacteria. Meningoencephalomyelitis [MEM] is a form of meningoencephaliits which also affects the spinal cord. In a June 2018 article, a team of PennVet clinicians diagnosed meningoencephalomyelitis caused by the bacteria Pasteurella multocida in a 5-year-old cavalier King Charles spaniel. (Meningoencephalomyelitis [MEM] is inflammation of the brain, including its protective membranes, and of the spinal cord, caused by a bacteria.) The dog had severe periodontal disease, with contact ulceration and possible necrotizing stomatitis. Her symptoms included fever, lethargy, inappetence, and multifocal neurologic signs, mainly dull mentation. Based upon examination of her cerebrospinal fluid (CSF) and blood culture, and her response to therapy (anti-emetics and gastroprotectants, an opioid for analgesia, and dexamethasone sodium phosphate as an antiinflammatory), P. multocida meningoencephalomyelitis was diagnosed. They opine that the severe periodontal disease led to a bacteremia causing hematogenous seeding of a bacterial meningitis originating at the disrupted blood-spinal cord barrier.They concluded:
"In the future, be aware that a fever with multifocal neurologic signs and severe periodontal disease in a canine patient may suggest a P. multocida infection and both CSF and blood cultures can be submitted for confirmation."
RETURN TO TOP
Possible Systemic Disorders
• Endocarditis: While endocarditis is a different disease from the mitral valve disease (MVD) affecting cavaliers (also called endocardiosis), this infectious disorder damages the heart valves and may extend to blood clots in the blood vessels.
• Cerebellar Infarcts (Strokes): Oral bacterias have been linked to cerebral infarctions.
• Meningoencephalomyelitis: In a June 2018 article, a team of PennVet clinicians diagnosed meningoencephalomyelitis caused by the bacteria Pasteurella multocida in a 5-year-old female cavalier with severe periodontal disease, with contact ulceration and possible necrotizing stomatitis. Meningoencephalomyelitis (MEM) is inflammation of the brain, including its protective membranes, and of the spinal cord, caused by a bacteria. Her symptoms included fever, lethargy, inappetence, and multifocal neurologic signs, mainly dull mentation. Based upon examination of her cerebrospinal fluid (CSF) and blood culture, and her response to therapy (anti-emetics and gastroprotectants, an opioid for analgesia, and dexamethasone sodium phosphate as an antiinflammatory), P. multocida meningoencephalomyelitis was diagnosed. They opined that the severe periodontal disease led to a bacteremia causing hematogenous seeding of a bacterial meningitis originating at the disrupted blood-spinal cord barrier.They concluded::
"In the future, be aware that a fever with multifocal neurologic signs and severe periodontal disease in a canine patient may suggest a P. multocida infection and both CSF and blood cultures can be submitted for confirmation."
• Diabetes Mellitus: There is a possible connection between orally-sourced inflammation and poor control of diabetes mellitus. See, for example, this January 2024 article.
• Kidney Disease: A kidney disease -- glomeruloneohriis -- is considered a potential consequence of chroiric bacteria associated with periodontal disease.
• Liver Disease: Bacteria from PD are a suspected cause of some hepatic disorders in dogs, including hepatitis and hepatic parenchyrnal inflammation.
RETURN TO TOP
Treatment
- Daily Brushing
- Antibiotics
- Food Supplements
- Periodic Cleaning Procedures
- Closed Root Planing
- Periodontal Flap Surgery
- Periodontal Tissue Regeneration
- Extraction
- Anesthesia-Free Dentistry
- Bone Chewing
The key to periodontal therapy is plaque control. Periodontal disease can be prevented by daily home care. See "What You Can Do" below. If the plaque already has taken hold of the dog's teeth and gums, causing gingivitis, then if the plaque is removed, it will in turn remove the gingivitis, allowing the return to a healthy tooth.
Watch this video about how to train your dog (and yourself) to brush its teeth.
Veterinary dental specialists recommend that small and other at-risk
breeds, particularly the cavalier King Charles spaniel, have their first
professional dental cleaning at nine to twelve months of age, followed
by periodic professional cleanings every six to nine month s thereafter.
These are intended to be preventative procedures as well as treatments
if affected teeth need to be surgically cared for or removed. Oral procedures
 under full anesthesia
(anaesthesia) are required for all levels of veterinary care beyond
daily home care.
under full anesthesia
(anaesthesia) are required for all levels of veterinary care beyond
daily home care.
An Internet search engine for finding board certified veterinary dentists is linked here.
RETURN TO TOP
Daily Brushing
In this February 2024 article, Turkish veterinarian Tülay Koneçoğlu Sütlü reported: "Regular dental brushing has been found to support significant treatment in patients who are still in the early stages of the disease, even while differences in the antibiotics used in medical treatment do not yield substantial differences in outcomes."
RETURN TO TOP
Antibiotics
Since periodontal disease in dogs is caused by bacteria, particularly P. gulae, antibacterial treatments have been tested. They include pradofloxacin, a combination of clindamycin and interferon alpha (IFN-a), COR388, and polyphosphates (polyP).
RETURN TO TOP
Food Supplements
Coenzyme Q10 (CoQ10)
-- Daily supplementation of
CoQ10 (ubiquinone or ubiquinol) has
been reported to be beneficial both as boosting resistance to, and
treatment for, periodontal disease. Dosages from 30 mg. to of
 100 mg. of
CoQ10 twice daily has been found to be well tolerated. See this
January
1983 article and this
October 2021 article.
100 mg. of
CoQ10 twice daily has been found to be well tolerated. See this
January
1983 article and this
October 2021 article.
Ascophyllum nodosum -- This is a powered seaweed in the kelp algae family which, when given to dogs orally on a daily basis, has been found in this June 2021 article and this September 2023 article to reduce the formation of plaque and tartar significantly when compared to control groups of dogs. ProDen PlaqueOff Powder for Pets is a brand that has been used in veterinary studies of this supplement.
1-Tetradecanol complex (1-TDC)
is a mixture of
monounsaturated fatty acids (MUFAs) which have been found effective in
reducing chronic inflammation in the gums of humans, rabbits, and cats.
In
the cat study, gel
 capsules containing 525 mg of 1-TDC were squeezed
onto the affected gums of cats with moderate-to-severe periodontal
disease daily for six weeks. At the end of the study, the researchers
reported finding "significant reductions in all parameters of clinical
periodontal disease", which included "clinical attachment level",
"gingival index", and "bleeding on probing". There also was a decrease in
tooth mobility in the 1-TDC group cats, but it was not statistically
significant. They acknowledged that the "underlying mechanisms of action
of 1-TDC is still not elucidated". They concluded that daily 1-TDC
treatment of periodontal disease in cats should be considered to manage
the disorder. Thus far, we have found no similar studies including dogs.
capsules containing 525 mg of 1-TDC were squeezed
onto the affected gums of cats with moderate-to-severe periodontal
disease daily for six weeks. At the end of the study, the researchers
reported finding "significant reductions in all parameters of clinical
periodontal disease", which included "clinical attachment level",
"gingival index", and "bleeding on probing". There also was a decrease in
tooth mobility in the 1-TDC group cats, but it was not statistically
significant. They acknowledged that the "underlying mechanisms of action
of 1-TDC is still not elucidated". They concluded that daily 1-TDC
treatment of periodontal disease in cats should be considered to manage
the disorder. Thus far, we have found no similar studies including dogs.
RETURN TO TOP
Periodic Cleaning Procedures
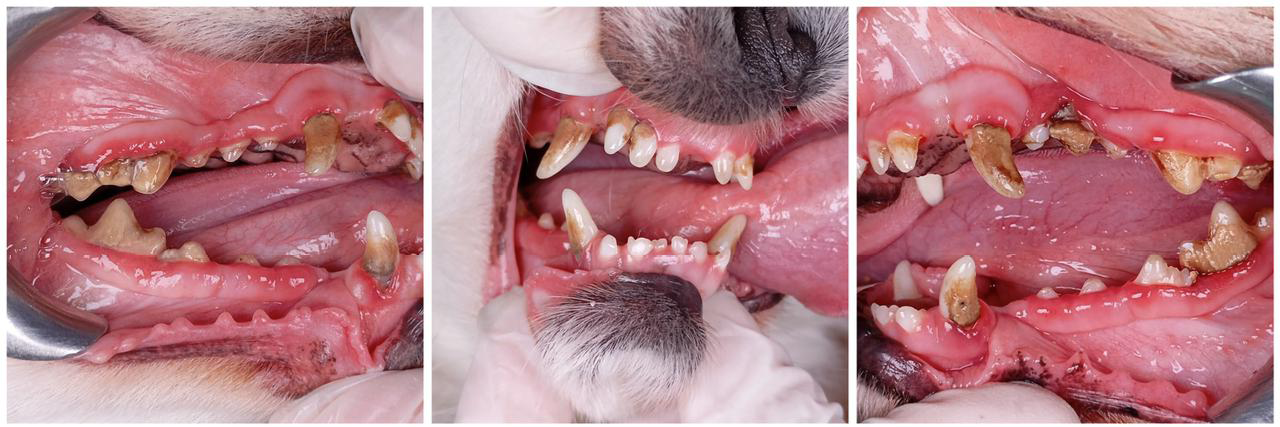
Periodic, thorough veterinary teeth and gum cleaning procedures under anesthesia are recommended, both as a preventative when the early stages of PD are detected, and especially after the onset of periodontitis. These Before & After photos, below, of a cleaning procedure of a cavalier are from this January 2025 article:

Preparation of the dog at home is essential before the dental procedure. Since the dog will be under anesethesia, no food should be offered after the evening before the treatment date. A sterile environment also is essential, since bacteria getting into the gums and the blood stream will lead straight to the heart. Therefore, many veterinarians advise dog owners to bathe their dogs at least once or twice in the days leading up to the date of the procedure, using an antiseptic shampoo such as VetraSeb CeraDerm.
The veterinarian probably will prescribe an oral antibiotic
medication to be given to the dog periodically, beginning the day before
the cleaning procedure. These pills will continue to be given for a
period of time after the dog returns home. The concern is that bacteria
in the dog's mouth, prior to and during the cleaning, may enter the
bloodsteam and cause systemic damage. However, in a
November 2023 article in which 13 healthy dogs had teeth removed
during a dental procedure, and did not receive any antibiotics,
begiining two weeks prior to the cleaning or afterwards, the researchers
found that any bacteria which appeared in their bloodstreams during and
following the cleaning had cleared from their blood without antibiotic
therapy. They
 concluded "that systemic antibiotic usage is not warranted
for severe periodontal disease where an episode of transient bacteremia
is produced from SRP and dental extractions in an otherwise healthy
patient."
concluded "that systemic antibiotic usage is not warranted
for severe periodontal disease where an episode of transient bacteremia
is produced from SRP and dental extractions in an otherwise healthy
patient."
Before the cleaning, but after the dog is placed under anesthesia, a full-mouth set of x-rays should be obtained. Only x-rays below the gum lines will show the extent of damage to the roots of the teeth and any bone loss. For example, the black areas around the roots of the teeth in this x-ray (right) are hollow from bone loss due to periodontal disease.
The veterinarians' cleaning process includes:
• Pre-anesthesia examination and work-up
• Proper anesthesia and monitoring by a trained veterinary professional
• Antiseptic (chlorhexidine) rinse (to decrease bacterial load)
• Supra-gingival scaling (cleaning the visible crown)
• Subgingival scaling (under the gumline cleaning - the most important step)
• Thorough polishing
• Sulcal lavage
• Oral exam and charting
• Dental radiographs
• Treatment planning and any additional therapy
• Application of a barrier sealant where appropriate
RETURN TO TOP
Closed Root Planing
Periodontal disease (PD) is an inflammatory disease of the gums. It is defined as periodontal pockets greater than 3 mm in depth. Pockets between 3 and 6 mm can be treated by "closed root planing" and placement of a long-acting antibiotic, if the tooth has not become loose (mobile). Root planing means using dental instruments to scrape the tooth's roots, which are below the normal gum line but which have become bare and visible due to recession of the gums. By "closed", it means that the scraping is performed without having to surgically cut the gum away to access the roots.
If the pockets are too deep -- deeper than 6 mm -- or if furcation has occurred, closed root planing alone will be insufficient to avoid contnued infection of the teeth.
RETURN TO TOP
 Periodontal
Flap Surgery
Periodontal
Flap Surgery
If the pockets exceed 6 mm or furcation has occurred, then "periodontal flap surgery" is required. This procedure entails cutting into the gum, laying the gum flap back to see the bare tooth and roots and bone, to remove the plaque deep down below the gumline, and perhaps add bone-grafting material before sutchering the gum back in place. (See the flap surgery photo from dvm360, at right.)
RETURN TO TOP
Periodontal Tissue Regeneration
Following periodontl flap surgery, a repair process known as periodontal tissue regeneration or guided tissue regeneration (GTR) may be performed to re-establish attachment of cementum to alveolar bone. A liquid implant biomaterial made of porcine gelatin, produced from pig collagen is applied to serve as a type of tissue scaffold to encourage regrowth (regeneation) of the periodontal ligament cells to repopulate along the root surface in the pocket to encourag successfull healing.
RETURN TO TOP
Extraction
If the PD has progressed to the point of the tooth becoming loose, that tooth must be extracted. Tooth extraction is the one true cure of PD.
RETURN TO TOP
Anesthesia-Free Dentistry
"Anesthesia-free" dentistry -- essentially partial cleanings of the crowns of the teeth of conscious patients -- generally are inadequate because that form of treatment cannot do a thorough job of examining and cleaning the periodontal pockets and examining the roots and alveolar bone. While the visible part of the tooth -- the crown -- may be discolored due to plaque turning into tartar, that does not lead to periodontal disease. It is the area of the tooth below the gumline where gingivitis starts and then becomes periodontitis.
In an October 2025 article, the effectiveness of anesthesia-free dentistry (AFD) was compared to anesthetic dentistry for treatment of periodontal disease in 46 dogs, including 2 cavaliers. Periodontal diagnostic test strips (PDTS) scores were used to compare the results of the two forms of treatments -- 23 dogs in each group. The investigators report finding that the mean PDTS score was significantly lower at recheck examination after anesthetic dentistry for both groups. The mean initial PDTS score did not differ significantly between groups; however, the mean PDTS score at recheck examination was significantly lower for dogs after an anesthetized dental procedure (0.087; range, 0 to 1) versus AFD (4.35; range, 3 to 5). They concluded that, "No medical benefit was provided by AFD."
RETURN TO TOP
Bone Chewing
 Giving
the dog a bone is not the answer to either preventing or treating
periodontal disease. Roughly 24% of dogs diagnosed with dental disorders have fractureed
teeth, mostly attributable to bone chewing. Broken teeth cause pain and
usually lead to infection, especially if the
inner pulp is exposed. (See photo at right of exposed pulp in a
broken tooth.) Infection in turn may lead to abscesses and jaw bone
weakness.
Giving
the dog a bone is not the answer to either preventing or treating
periodontal disease. Roughly 24% of dogs diagnosed with dental disorders have fractureed
teeth, mostly attributable to bone chewing. Broken teeth cause pain and
usually lead to infection, especially if the
inner pulp is exposed. (See photo at right of exposed pulp in a
broken tooth.) Infection in turn may lead to abscesses and jaw bone
weakness.
When veterinary specialist Dr. Jan Bellows was asked, "How can I prevent my dog from fracturing more teeth?", he responded: "Examine your dog's treats and chew toys. Eliminate any bones, antlers, cow hoofs, nylon chews, and pizzle sticks. Throw out chews or toys that do not readily bend."
Bone chewing also cannot treat periodontal disease (PD), because no amount of bone chewing can reach below the surface of the dog's gums, which is where PD is located. See What is Periodontal Disease, above.
In a February 2020 article, a team of Brazilian veterinary dental researchers studied the effects of twelve Beagles chewing either sterile cortical (hard) bovine femur bones or sterile spongy bovine femur bones over a two week period, to evaluate the effect of bone chewing on the dental roots, enamel, and gingiva of the dogs. They report that both types of bones "were highly effective in removing dental calculus" and gingival inflammation reduction, with the spongy bones being more effective than the hard ones. Dental calculus was completely removed from the first and second premolars and molars in less than three days. No lesions or teeth root and enamel fracture, or esophageal or intestinal obstructions were observed. However, the spongy showed some gingival lesions and bone remnants between the dogs' teeth. Gingival lesions were caused by the daily and continuous supply of new pieces of bone for the 13 days. However, the bones failed to cure or even partially treat periodontal disease, which is a below-the-gumline disorder. They stated:
"Although there was an improvement in the visual appearance of the gum, there was no reduction in plaque and calculus under the gumline. The maintenance of subgingival [below the gumline] plaque and calculus is the etiological factor of loss of dental adhesion to its alveolus, characteristic to periodontal disease. Thus, bones are not efficient in removing plaque and calculus under the gumline, they are only able to remove it on the crown." (Emphasis added.)
In a January 2016 article, 8 Beagles were tested twice by giving them bovine bones to chew. In the first test, the dogs each were given a raw hard bone from the bovine femur each day for 12 days. In the second test, which was started 7 months after the end of the first test, the same dogs each were given a raw spongy bone, also from the femur, each day for 20 days. The Brazilian investigators report finding that the spongy bones "removed calculus [from the teeth] in the short term." They also report that none of the 8 Beagles suffered any broken teeth. However, they did not evaluate any injuries that may have occurred on the gingiva, enamel, and roots of the dogs' teeth. They also did not discuss the effects of the bone chewing on the dogs' gums at all. They concluded:
"Compared with the other dental calculus control methods already discussed, except for tooth brushing, bone supplementation in our study showed similar, or better, effect than in studies of polyphosphate use and rawhide chews."
While this January 2016 study may give some support to bone chewing to reduce calculus on the dogs' teeth, its downsides are that: (a) it consisted of only 8 dogs, and of only one breed; (b) the bone chewing had no stated effect whatsoever upon the gums,where peridontal disease exists; and (c) the results were not as successful as daily tooth brushing.
RETURN TO TOP
Genetics
While PD has not been shown to be more common in the cavalier than in other breeds, in an April 2014 study, Portugese veterinarians, searching the genetics of canine periodontal disease, discovered that variants of the interleukin-10 gene, particularly interleukin-10 (IL-10), is "highly polymorphic with genetic variants that may be important in PD susceptibility." Previous studies of IL-10 in the CKCS suggest that it may play a role in determining the cavaliers' susceptibility to diabetes.
RETURN TO TOP
Breeders' Responsibilities
Since cavaliers are more susceptible to this dental and gum disorder called periodontal disease (PD) than any other dog breed, breeders should educate their buyers about the vital importance of daily dental home care and how best to perform it.
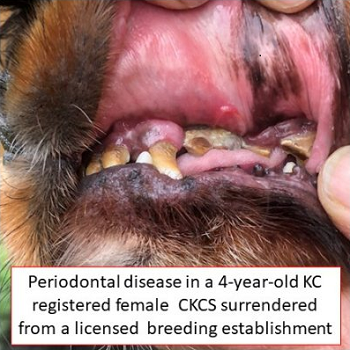 At
the March 2024 BSAVA 2024 conference, UK researchers found that among
177 cavaliers surrendered to a cavalier rescue group, retired breeding
stock cavaliers surrendered by breeders had the worst cases of dental
disease, of which 92% required tooth extractions, with 76.3% requiring
21 or more teeth removed. They presented
a poster examining the reasons 177 cavalier King Charles spaniels
were surrendered by their owners to a UK canine rescue group, Bliss
Cavalier Rescue. The data was collected from a combination of
questionnaires, health checklists, veterinary medical histories, and
veterinary examinations following surrender. At the date of surrender,
these cavaliers by age 6 years had an average of 6 physical health
conditions (excluding anxiety, obesity, and underweight), referred to in
the study as multi-morbidities. The second most common health condition
(after painful Chiari-like malformation)
was dental disease requiring extractions, numbering 121 cavaliers
(68.45%). The researchers highlighted the details regarding dental
disease. The cavaliers surrendered by breeders had the average age of
5.5 years, and 94.4% of those breeders were registered with the UK
Kennel Club.
At
the March 2024 BSAVA 2024 conference, UK researchers found that among
177 cavaliers surrendered to a cavalier rescue group, retired breeding
stock cavaliers surrendered by breeders had the worst cases of dental
disease, of which 92% required tooth extractions, with 76.3% requiring
21 or more teeth removed. They presented
a poster examining the reasons 177 cavalier King Charles spaniels
were surrendered by their owners to a UK canine rescue group, Bliss
Cavalier Rescue. The data was collected from a combination of
questionnaires, health checklists, veterinary medical histories, and
veterinary examinations following surrender. At the date of surrender,
these cavaliers by age 6 years had an average of 6 physical health
conditions (excluding anxiety, obesity, and underweight), referred to in
the study as multi-morbidities. The second most common health condition
(after painful Chiari-like malformation)
was dental disease requiring extractions, numbering 121 cavaliers
(68.45%). The researchers highlighted the details regarding dental
disease. The cavaliers surrendered by breeders had the average age of
5.5 years, and 94.4% of those breeders were registered with the UK
Kennel Club.
In a July 2025 article, 4,771 Finnish dogs' medical records were reviewed to determine early life factors contributing to reports of dental calculus (DC) and its risks and protective factors. They reported:
"Our research indicated that dogs fed a non-processed meat-based diet during the weaning period, puppyhood, and adolescence, which corresponds to the age range of 1 month to 1 or 1.5 years, were associated with a significantly lower risk of developing DC later in life. Conversely, dogs consumed an ultra-processed carbohydrate-based diet during the same periods [weaning, puppyhood, and adolescence, respectively] was associated with a significantly higher risk."
RETURN TO TOP
Other Dental Disorders
Other disorders observed in the mouths of some cavaliers include abnormal bites (malocclusion) and overly large tongues (macroglossia). While they are not caused by periodontal disease or directly realated to it, these disorders may contribute to PD, either as a cause of a worsening of the condition.
Malocclusion (Abnormal Bite)
 Malocclusion
is veterinary-ese for an abnormal bite, a condition of the upper and
lower sets of teeth not aligning properly when the jaw is closed. It may
be an over-bite (see image at right), an under-bite, or an
asymmetrical bite. It is a common problem among dogs and particularly
among cavalier King Charles spaniels. It can be hereditary or acquired
and can be influenced by a variety of internal or environmental factors,
and also trauma or delayed loss of deciduous (baby) teeth.
Malocclusion
is veterinary-ese for an abnormal bite, a condition of the upper and
lower sets of teeth not aligning properly when the jaw is closed. It may
be an over-bite (see image at right), an under-bite, or an
asymmetrical bite. It is a common problem among dogs and particularly
among cavalier King Charles spaniels. It can be hereditary or acquired
and can be influenced by a variety of internal or environmental factors,
and also trauma or delayed loss of deciduous (baby) teeth.
Depending upon the severity of the abnormal bite, all sorts of damage can result, such as:
• difficulty chewing food
• teeth piercing the soft gums and causing trauma and ulceration
• tooth-on-tooth wear and fractures
• premature tooth loss
• rotated, fused, or unerupted teeth
• temporomandibular joint dysfunction.
In problematic cases, treatment is required, varying from orthodontures to surgery.
RETURN TO TOP
Retained Baby Teeth
 The puppy's 28 baby (deciduous) teeth normally start dropping out
(exfoliate) at between three to six months of age, as their permanent
teeth first appear. The erupting permanent teeth put pressure on the
baby teeth, causing their roots to be resorbed and the baby teeth to
loosen and drop. If the emerging permanent teeth do not follow their
correct paths, this loosening process may not occur, and the baby teeth
do not fall out, resulting in their retention, called persisent
deciduous teeth (PDT). The most common PDTs are the canines.
The puppy's 28 baby (deciduous) teeth normally start dropping out
(exfoliate) at between three to six months of age, as their permanent
teeth first appear. The erupting permanent teeth put pressure on the
baby teeth, causing their roots to be resorbed and the baby teeth to
loosen and drop. If the emerging permanent teeth do not follow their
correct paths, this loosening process may not occur, and the baby teeth
do not fall out, resulting in their retention, called persisent
deciduous teeth (PDT). The most common PDTs are the canines.
PDT can result in serious conditions for the dog, such as malocclusion due to the inability of the incoming permanent teeth to reach their proper positioning, and especially crowding, which then leads to hastening the formation of plaque and progression to periodontal inflammation. In a March 2024 article, in which the medical records of nearly 3 million dogs in the United States were studied over a 5 year period, the investigators found that the cavalier King Charles spaniel was second only to the pug in prevalence of PDT.
 PDTs should be extracted promptly, to avoid likely periodontal and
malocclusion consequences. During the extraction procedure, care must be
taken to not damage the incoming permanent teeth, particularly to the
immature enamel, which cannot be repaired.
PDTs should be extracted promptly, to avoid likely periodontal and
malocclusion consequences. During the extraction procedure, care must be
taken to not damage the incoming permanent teeth, particularly to the
immature enamel, which cannot be repaired.
In a March 2018 case study at San Juan Veterinary Clinic in Colorado, the clinicians inserted temporary orthodontic braces on an 8-month-old cavalier, Oscar, to force the displaced permanent canine tooth (in the photo above) to move back to its normal postion. (See photo at right.)
In a February 2024 article, two UK dentistry specialists reported a case study of a 23-month-old cavalier with the root of its left upper baby canine tooth (#204 on the chart above) which had grown into the pulp of its permanent canine tooth, preventing the permanent tooth's full development. At age 6 months, the cavalier's canine teeth had been extracted due to their failure to fall out naturally. Seventeen months later, the permanent left maxillary (upper) canine tooth was found to have stopped developing. X-rays showed that the root of the baby tooth remained and was inside of the pulp of the immature permanent tooth. The permanent tooth had to be removed. The authors concluded by recommending that this unusual complication should be considered when extracting peristent baby teeth.
RETURN TO TOP
Macroglossia (Enlarged Tongue)
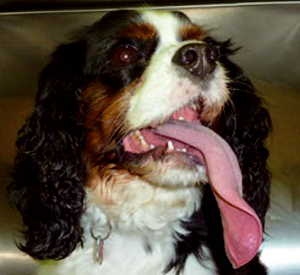 Cavaliers have been known to have excessively large tongues, resulting
in the dogs' inability to containt their full tongues in their closed
mouths. The veterinary-ese for this disorder is called macroglossia. In
a November 2011 article, Dr. Gerhard Putter reported the case study of a
5-year-old male CKCS with such a condition. During panting, the dog's
tongue protruded about 10 cm from the left side of the mouth. (See
image at right.) Any attempt by the dog to withdraw the tongue into
the mouth caused the left upper lip to be drawn into the mouth. It was
therefore not possible for the dog to return the tongue to its normal
intraoral position. This caused the surface of the left upper lip to be
constantly wet with saliva. Generalised moderate calculus associated
with slight to moderate gingivitis was present. The pressure from the
deviated tongue on the left maxillary as well as mandibular premolars
has caused the deviation of these teeth laterally. This also explains
the greater rotation and deviation of the rostral aspect of the left
mandible because more pressure was exerted by the tongue on these teeth.
At some stage during the progression of the condition, the left upper
lip has become involved. The hair on the upper lip appears to have
prevented complete retraction of the tongue into the mouth and to have
caused the lip to be drawn into the left side of the oral cavity. The
owner opted not to consider surgical repair of the malocclusion and the
deviation of the left mandible.
Cavaliers have been known to have excessively large tongues, resulting
in the dogs' inability to containt their full tongues in their closed
mouths. The veterinary-ese for this disorder is called macroglossia. In
a November 2011 article, Dr. Gerhard Putter reported the case study of a
5-year-old male CKCS with such a condition. During panting, the dog's
tongue protruded about 10 cm from the left side of the mouth. (See
image at right.) Any attempt by the dog to withdraw the tongue into
the mouth caused the left upper lip to be drawn into the mouth. It was
therefore not possible for the dog to return the tongue to its normal
intraoral position. This caused the surface of the left upper lip to be
constantly wet with saliva. Generalised moderate calculus associated
with slight to moderate gingivitis was present. The pressure from the
deviated tongue on the left maxillary as well as mandibular premolars
has caused the deviation of these teeth laterally. This also explains
the greater rotation and deviation of the rostral aspect of the left
mandible because more pressure was exerted by the tongue on these teeth.
At some stage during the progression of the condition, the left upper
lip has become involved. The hair on the upper lip appears to have
prevented complete retraction of the tongue into the mouth and to have
caused the lip to be drawn into the left side of the oral cavity. The
owner opted not to consider surgical repair of the malocclusion and the
deviation of the left mandible.
RETURN TO TOP
What You Can Do
 The key to periodontal therapy is plaque control. Beginning at 6 months, daily cleaning of the dog's teeth and gums is critical to avoiding
periodontal disease. Plaque can attach to the teeth within twenty-four
hours if not subject to daily cleaning. Therefore, the goal of daily
care is to reduce the amount of bacteria on the teeth, thereby
decreasing gingival inflammation and avoiding PD. Since cavaliers are an
"at-risk" breed for PD, it is critical that homecare be started early.
The key to periodontal therapy is plaque control. Beginning at 6 months, daily cleaning of the dog's teeth and gums is critical to avoiding
periodontal disease. Plaque can attach to the teeth within twenty-four
hours if not subject to daily cleaning. Therefore, the goal of daily
care is to reduce the amount of bacteria on the teeth, thereby
decreasing gingival inflammation and avoiding PD. Since cavaliers are an
"at-risk" breed for PD, it is critical that homecare be started early.
In this February 2024 article, Turkish veterinarian Tülay Koneçoğlu Sütlü reported: "Regular dental brushing has been found to support significant treatment in patients who are still in the early stages of the disease, even while differences in the antibiotics used in medical treatment do not yield substantial differences in outcomes."
When properly performed, tooth brushing is the most effective method of controlling plaque. See this May 2015 article. The movement of the brush is a key to controlling the plaque. The owner should begin training the dog to accept the brush and its movement as early as possible, making the process a learned behavior. Alternatively, applying tooth paste or other dental ointments is second best to actual daily brushing. See this April 2016 article. Be sure to brush along the gum lines and not just the crowns of the teeth.
Watch this video about how to train your dog (and yourself) to brush its teeth.
Avoid feeding processed dog foods (like kibble, dry foods). In a July 2025 article, 4,771 Finnish dogs' medical records were reviewed to determine early life factors contributing to reports of dental calculus (DC) and its risks and protective factors. They reported:
"Our research indicated that dogs fed a non-processed meat-based diet during the weaning period, puppyhood, and adolescence, which corresponds to the age range of 1 month to 1 or 1.5 years, were associated with a significantly lower risk of developing DC [dental calculus] later in life. Conversely, dogs consumed an ultra-processed carbohydrate-based diet during the same periods [weaning, puppyhood, and adolescence, respectively] was associated with a significantly higher risk."
Daily supplementation of
Coenzyme Q10 (CoQ10) has
been reported to be beneficial both as boosting
 resistance to, and
treatment for, periodontal disease. Dosages from 30 mg. to of 100 mg. of
resistance to, and
treatment for, periodontal disease. Dosages from 30 mg. to of 100 mg. of
 CoQ10 twice daily has been found to be well tolerated. See this
January
1983 article and this
October 2021 article.
CoQ10 twice daily has been found to be well tolerated. See this
January
1983 article and this
October 2021 article.
Ascophyllum nodosum -- This is a powered seaweed in the kelp algae family which, when given to dogs orally on a daily basis, has been found in this June 2021 article and this September 2023 article to reduce the formation of plaque and tartar significantly when compared to control groups of dogs. ProDen PlaqueOff Powder for Pets is a brand that has been used in veterinary studies of this supplement.
Also, consider the daily application of
1-Tetradecanol complex (1-TDC)
on the gums of
 your dog. 1-TDC is a mixture of
monounsaturated fatty acids (MUFAs) which have been found effective in
reducing chronic inflammation in the gums of humans, rabbits, and cats.
In
the cat study, gel capsules containing 525 mg of 1-TDC were squeezed
onto the affected gums of cats with moderate-to-severe periodontal
disease daily for six weeks. At the end of the study, the researchers
reported finding "significant reductions in all parameters of clinical
periodontal disease", which included "clinical attachment level",
"gingival index", and "bleeding on probing". There also was a decrease in
tooth mobility in the 1-TDC group cats, but it was not statistically
significant. They acknowledged that the "underlying mechanisms of action
of 1-TDC is still not elucidated". They concluded that daily 1-TDC
treatment of periodontal disease in cats should be considered to manage
the disorder. Thus far, we have found no similar studies including dogs.
your dog. 1-TDC is a mixture of
monounsaturated fatty acids (MUFAs) which have been found effective in
reducing chronic inflammation in the gums of humans, rabbits, and cats.
In
the cat study, gel capsules containing 525 mg of 1-TDC were squeezed
onto the affected gums of cats with moderate-to-severe periodontal
disease daily for six weeks. At the end of the study, the researchers
reported finding "significant reductions in all parameters of clinical
periodontal disease", which included "clinical attachment level",
"gingival index", and "bleeding on probing". There also was a decrease in
tooth mobility in the 1-TDC group cats, but it was not statistically
significant. They acknowledged that the "underlying mechanisms of action
of 1-TDC is still not elucidated". They concluded that daily 1-TDC
treatment of periodontal disease in cats should be considered to manage
the disorder. Thus far, we have found no similar studies including dogs.
Note that bone chewing has not been shown to be effective in either preventing or treating periodontal disease. Chewing on bones also can result in tooth fractures. See the Bone Chewing section above.
 Since
cavaliers are more susceptible to periodontal disease than are most
breeds, owners should consider having their CKCSs examined by dental
specialists. An Internet search engine for finding board certified veterinary
dentists is
linked here.
Since
cavaliers are more susceptible to periodontal disease than are most
breeds, owners should consider having their CKCSs examined by dental
specialists. An Internet search engine for finding board certified veterinary
dentists is
linked here.
Research News
July 2025: A case study of periodontal disease in a cavalier King Charles spaniel. In a January 2025 article, Brazilian dental specialists report on the diagnosis of and treatment of a cavalier King Charles spaniel with periodontal disease. The dog had halitosis, the presence of dental calculus and oral bleeding after brushing of dog's teeth. The dog's owners brushed the teeth only sporadically. The clinicians observed an accumulation of dental calculus and associated gingivitis. Some of the teeth were loose, indicating advanced periodontal disease. They performed computed tomography with 3D imaging, which revealed bone loss of supporting tissues. Underr anesthesia, the dog's dental calculus was removed, loose teeth were extractred, and all affected teeth were polished to remove stains. The clinicians recommended antibiotics (clindamycin, metronidazole and spiramycin) started 3 days before surgery and 7 days afterwards, to reduce inflammation, reduce bleeding caused by scraping, reduce halitosis, and reduce formation of biofilm and dental calculus.
August 2024:
Turkish study finds periodontal disease in cavaliers is
associated with being fed dry foods.
 In a
February 2024 thesis, Turkish
veterinarian Tülay Koneçoğlu Sütlü (right) evaluated periodontal disease in 16 dogs, including
3 cavalier King Charles spaniels (18.75%). She observed a trend among
dogs being fed dry foods to develop periodontal disease. All dogs in the
study had halitosis. Also, 6 out of 16 dogs (37.5%) had difficulty
eating dry food and dropped the food from their mouths. She concluded
that:
In a
February 2024 thesis, Turkish
veterinarian Tülay Koneçoğlu Sütlü (right) evaluated periodontal disease in 16 dogs, including
3 cavalier King Charles spaniels (18.75%). She observed a trend among
dogs being fed dry foods to develop periodontal disease. All dogs in the
study had halitosis. Also, 6 out of 16 dogs (37.5%) had difficulty
eating dry food and dropped the food from their mouths. She concluded
that:
"Regular dental brushing has been found to support significant treatment in patients who are still in the early stages of the disease, even while differences in the antibiotics used in medical treatment do not yield substantial differences in outcomes. The study has revealed the significance of tooth brushing, particularly for pet owners with dogs and cats. Regular tooth brushing habit is necessary to protect against diseases, and it can be therapeutic in the early stages of the disease."
March 2024:
UK breeders surrendered retired breeding cavaliers to rescue
group with worst cases of dental disease.
 At
the March 2024 BSAVA 2024 conference, UK researchers Rebecca Mosley,
Tena Kras, Clare Buxton, Felipe Zabaneh Rodal, Peter Buxton, and Clare
Rusbridge presented a
poster examining the reasons 177 cavalier King Charles spaniels were
surrendered by their owners to a UK canine rescue group,
Bliss Cavalier
Rescue. The data was collected from a combination of questionnaires,
health checklists, veterinary medical histories, and veterinary
examinations following surrender. At the date of surrender, these
cavaliers by age 6 years had an average of 6 physical health conditions
(excluding anxiety, obesity, and underweight), referred to in the study
as multi-morbidities. The second most common health condition (after
painful Chiari-like malformation) was
dental disease requiring extractions, numbering 121 cavaliers (68.45%).
The researchers highlighted the details regarding dental disease. They
found that retired breeding stock cavaliers surrendered by breeders had
the worst cases of dental disease, of which 92% required tooth
extractions, with 76.3% requiring 21 or more teeth removed. The
cavaliers surrendered by breeders had the average age of 5.5 years, and
94.4% of those breeders were registered with the UK Kennel Club.
At
the March 2024 BSAVA 2024 conference, UK researchers Rebecca Mosley,
Tena Kras, Clare Buxton, Felipe Zabaneh Rodal, Peter Buxton, and Clare
Rusbridge presented a
poster examining the reasons 177 cavalier King Charles spaniels were
surrendered by their owners to a UK canine rescue group,
Bliss Cavalier
Rescue. The data was collected from a combination of questionnaires,
health checklists, veterinary medical histories, and veterinary
examinations following surrender. At the date of surrender, these
cavaliers by age 6 years had an average of 6 physical health conditions
(excluding anxiety, obesity, and underweight), referred to in the study
as multi-morbidities. The second most common health condition (after
painful Chiari-like malformation) was
dental disease requiring extractions, numbering 121 cavaliers (68.45%).
The researchers highlighted the details regarding dental disease. They
found that retired breeding stock cavaliers surrendered by breeders had
the worst cases of dental disease, of which 92% required tooth
extractions, with 76.3% requiring 21 or more teeth removed. The
cavaliers surrendered by breeders had the average age of 5.5 years, and
94.4% of those breeders were registered with the UK Kennel Club.
February 2024:
Cavalier's baby canine tooth root prevented development of its
permanent canine tooth.
 In
a
February 2024 article, two UK dentistry specialists (Charlie Tewson
[right], Simone Kirby) report a case study of a 23-month-old
cavalier King Charles spaniel with the root of its left upper baby
canine tooth (#204 on the chart above) which had
grown into the pulp of its permanent canine tooth, preventing the
permanent tooth's full development. At age 6 months, the cavalier's
canine teeth had been extracted due to their failure to fall out
naturally. Seventeen months later, the permanent left maxillary (upper)
canine tooth was found to have stopped developing. X-rays showed that
the root of the baby tooth remained and was inside of the pulp of the
immature permanent tooth. The permanent tooth had to be removed. The
authors conclude by recommending that this unusual complication should
be considered with extracting peristent baby teeth.
In
a
February 2024 article, two UK dentistry specialists (Charlie Tewson
[right], Simone Kirby) report a case study of a 23-month-old
cavalier King Charles spaniel with the root of its left upper baby
canine tooth (#204 on the chart above) which had
grown into the pulp of its permanent canine tooth, preventing the
permanent tooth's full development. At age 6 months, the cavalier's
canine teeth had been extracted due to their failure to fall out
naturally. Seventeen months later, the permanent left maxillary (upper)
canine tooth was found to have stopped developing. X-rays showed that
the root of the baby tooth remained and was inside of the pulp of the
immature permanent tooth. The permanent tooth had to be removed. The
authors conclude by recommending that this unusual complication should
be considered with extracting peristent baby teeth.
December 2022:
Cavaliers ranked third among breeds with malaligned teeth in a
three-year California study.
 In
a
December 2022 article, three USA veterinary dental specialists
(Marissa Berman [right], Maria Soltero-Rivera, Amy J. Fulton
Scanlan) examined the records of 198 dogs presented to a California
veterinary dental clinic (VCA Encina Veterinary Medical Center) with
abnormal alignment (maloccusion) of either their baby teeth (deciduous)
or permanent teeth. There are two types of malocclusions: (1) skeletal,
which means that an abnormal jaw length results in a misalignment of the
teeth, and (2) dental, which occurs when one ore more teeth are out of
normal alignment, also called malpositioned teeth. In this California
study, which spanned from 2015 to 2018, the cavalier King Charles
spaniel, along with the poodle and Labrador retriever, comprised 50% of
the dogs with deciduous (baby teeth) malocclusions. The five most
commonly affected breeds with permanent malocclusions were the cavalier,
along with poodles, Labrador retrievers, chihuahuas, and pit bull
terriers.
In
a
December 2022 article, three USA veterinary dental specialists
(Marissa Berman [right], Maria Soltero-Rivera, Amy J. Fulton
Scanlan) examined the records of 198 dogs presented to a California
veterinary dental clinic (VCA Encina Veterinary Medical Center) with
abnormal alignment (maloccusion) of either their baby teeth (deciduous)
or permanent teeth. There are two types of malocclusions: (1) skeletal,
which means that an abnormal jaw length results in a misalignment of the
teeth, and (2) dental, which occurs when one ore more teeth are out of
normal alignment, also called malpositioned teeth. In this California
study, which spanned from 2015 to 2018, the cavalier King Charles
spaniel, along with the poodle and Labrador retriever, comprised 50% of
the dogs with deciduous (baby teeth) malocclusions. The five most
commonly affected breeds with permanent malocclusions were the cavalier,
along with poodles, Labrador retrievers, chihuahuas, and pit bull
terriers.
August 2021:
Cavaliers are found to have a "strong breed predisposition for
periodontal disease", in UK study.
 In
an
August 2021 article, UK researchers (D. G. O'Neill, C. E. Mitchell,
J. Humphrey, D. B. Church, D. C. Brodbelt [right], C. Pegram)
reviewed the veterinary records of a random sample of 22,333 dogs among
over 900,000 attending 784 clinics during 2016, to determine the breeds
with the greatest prevalence of having periodontal disease. They
measured the breeds by (a) prevalence of diagnosis, (b) increased odds,
and (c) breed predisposition. They report that the cavalier King Charles
spaniel ranked 4th (behind the greyhound, King Charles spaniel, and toy
poodle) in prevalence of diagnosis. The cavalier also came in 4th
(behind the toy poodle, King Charles spaniel, and greyhound) in
increased odds compared to crossbred dogs. They found that, overall,
periodontal disease is a common diagnosis in UK dogs, with one in eight
dogs diagnosed annually. They concluded that cavaliers have "a strong
breed predisposition for periodontal disease".
In
an
August 2021 article, UK researchers (D. G. O'Neill, C. E. Mitchell,
J. Humphrey, D. B. Church, D. C. Brodbelt [right], C. Pegram)
reviewed the veterinary records of a random sample of 22,333 dogs among
over 900,000 attending 784 clinics during 2016, to determine the breeds
with the greatest prevalence of having periodontal disease. They
measured the breeds by (a) prevalence of diagnosis, (b) increased odds,
and (c) breed predisposition. They report that the cavalier King Charles
spaniel ranked 4th (behind the greyhound, King Charles spaniel, and toy
poodle) in prevalence of diagnosis. The cavalier also came in 4th
(behind the toy poodle, King Charles spaniel, and greyhound) in
increased odds compared to crossbred dogs. They found that, overall,
periodontal disease is a common diagnosis in UK dogs, with one in eight
dogs diagnosed annually. They concluded that cavaliers have "a strong
breed predisposition for periodontal disease".
July 2021:
Cavaliers top the list of having periodontal disease among
medium-small breeds, 5-year US study shows.
 In
a
July 2021 article, investigators (C. Wallis [right], E.K.
Saito, C. Salt, L.J. Holcombe, N.G. Desforges) reviewed the medical
records of 2,841,038 dogs of 60 pure breeds of dogs at Banfield
veterinary clinics between 2010 and 2014 to find the breeds, age,
gender, neuter status, weight, and body condition score, and frequency
of dental treatment visits of all dogs diagnosed with periodontal
disease (PD), which included periodontal
pocket, gingival recession, attachment
loss percentages, and periodontitis.
In
a
July 2021 article, investigators (C. Wallis [right], E.K.
Saito, C. Salt, L.J. Holcombe, N.G. Desforges) reviewed the medical
records of 2,841,038 dogs of 60 pure breeds of dogs at Banfield
veterinary clinics between 2010 and 2014 to find the breeds, age,
gender, neuter status, weight, and body condition score, and frequency
of dental treatment visits of all dogs diagnosed with periodontal
disease (PD), which included periodontal
pocket, gingival recession, attachment
loss percentages, and periodontitis.
The 10 breeds with the highest prevalence of PD (Grades 1-4 combined) were: Greyhound (38.7%), Shetland sheepdog (30.6%), Papillon (29.7%), Toy poodle (28.9%), Miniature poodle (28.2%), Dachshund (28.1%), Bichon frise (27.9%), Cavalier King Charles spaniel (27.3%), American Eskimo dog (27.0%), and Cairn terrier (26.8%). ... Cavaliers had the highest probability of PD within the medium-small size category. The odds of a CKCS having PD was over 8 times that of a French bulldog. Additional risk factors for PD diagnosis included age, being overweight, and the length of time since the dog's last scaling and polishing of its teeth.
May 2021:
US study finds a link between dogs with periodontal disease and
canine cognitive dysfunction.
 In
an
April 2021 article, Drs. Curtis W. Dewey [right] and Mark
Rishniw report the results of a study of 21 aging (over 9 years of age)
dogs -- 11 diagnosed with canine cognitive dysfunction (CCD) and 10
(including one cavalier King Charles spaniel) control dogs. All 21 dogs
were visually examined and photographed for periodontal disease, which
was ranked mild, moderate, or severe. Owners of the dogs with CCD
completed questionnaires examining six variables: disorientation,
interactions-social, sleep/wake cycles, house soiling/ learning/ memory,
activity, and anxiety (DISHAA) to produce a score that determined their
dogs' degree of cognitive impairment or dysfunction. A team of 12
veterinarians evaluated the dogs' dental photographs and scored the
severity of periodontal disease on a scale of 0 to 4. They report that
scores of cognitive dysfunction correlated positively, but modestly,
with periodontal disease. They concluded that their study has identified
an association between visually categorized periodontal disease and CCD,
but that further and more detailed investigations are called for.
In
an
April 2021 article, Drs. Curtis W. Dewey [right] and Mark
Rishniw report the results of a study of 21 aging (over 9 years of age)
dogs -- 11 diagnosed with canine cognitive dysfunction (CCD) and 10
(including one cavalier King Charles spaniel) control dogs. All 21 dogs
were visually examined and photographed for periodontal disease, which
was ranked mild, moderate, or severe. Owners of the dogs with CCD
completed questionnaires examining six variables: disorientation,
interactions-social, sleep/wake cycles, house soiling/ learning/ memory,
activity, and anxiety (DISHAA) to produce a score that determined their
dogs' degree of cognitive impairment or dysfunction. A team of 12
veterinarians evaluated the dogs' dental photographs and scored the
severity of periodontal disease on a scale of 0 to 4. They report that
scores of cognitive dysfunction correlated positively, but modestly,
with periodontal disease. They concluded that their study has identified
an association between visually categorized periodontal disease and CCD,
but that further and more detailed investigations are called for.
March 2021:
Cavaliers are reported to be most susceptible to periodontal disease of
all dog breeds.
 In a
June
2021 article, in a not-yet published book (Breed Predispositions to
Dental and Oral Disease in Dogs), Dr. Brook A. Niemiec (right), a
veterinary dental specialist in California, has authored an extensive
review of periodontal disease and therapy in small and toy breeds. He
states that:
In a
June
2021 article, in a not-yet published book (Breed Predispositions to
Dental and Oral Disease in Dogs), Dr. Brook A. Niemiec (right), a
veterinary dental specialist in California, has authored an extensive
review of periodontal disease and therapy in small and toy breeds. He
states that:
"Cavalier King Charles Spaniels (CKCS) and Greyhounds are well known for significant periodontal disease. CKCS suffer from early onset periodontal disease, especially in the maxillary premolars (as they are similar to other brachycephalic breeds). There is quite often furcation exposure of these teeth as early as two years of age. Interestingly, it is quite common for them to have advance periodontal loss with minimum calculus and gingivitis. ... Both of these breeds are very difficult to manage due to the high genetic potential for the disease. They typically suffer from significant gingivitis and early bone loss with only minimal calculus.
"In general, these [brachycephalic] breeds do not appear to be more susceptible to periodontal disease than others of their size (with the exception of Cavalier King Charles Spaniels)."
February 2020:
Bone chewing fails to prevent or treat dogs' periodontal
disease, in a Brazilian study.
 In
a
February 2020 article, a team of Brazilian veterinary dental
researchers (Caroline Fredrich Dourado Pinto, Willian Lehr, Víviam Nunes
Pignone, Caio Peixoto Chain, Luciano Trevizan [right]) studied
the effects of twelve Beagles chewing either sterile cortical (hard)
bovine femur bones or sterile spongy bovine femur bones over a two week
period, to evaluate the effect of bone chewing on the dental roots,
enamel, and gingiva of the dogs. They report that both types of bones
"were highly effective in removing dental calculus" and gingival
inflammation reduction, with the spongy bones being more effective than
the hard ones. Dental calculus was completely removed from the first and
second premolars and molars in less than three days. No lesions or teeth
root and enamel fracture, or esophageal or intestinal obstructions were
observed. However, the spongy showed some gingival lesions and bone
remnants between the dogs' teeth. Gingival lesions were caused by the
daily and continuous supply of new pieces of bone for the 13 days.
However, the bones failed to cure or even partially treat periodontal
disease, which is a below-the-gumline disorder. They stated:
In
a
February 2020 article, a team of Brazilian veterinary dental
researchers (Caroline Fredrich Dourado Pinto, Willian Lehr, Víviam Nunes
Pignone, Caio Peixoto Chain, Luciano Trevizan [right]) studied
the effects of twelve Beagles chewing either sterile cortical (hard)
bovine femur bones or sterile spongy bovine femur bones over a two week
period, to evaluate the effect of bone chewing on the dental roots,
enamel, and gingiva of the dogs. They report that both types of bones
"were highly effective in removing dental calculus" and gingival
inflammation reduction, with the spongy bones being more effective than
the hard ones. Dental calculus was completely removed from the first and
second premolars and molars in less than three days. No lesions or teeth
root and enamel fracture, or esophageal or intestinal obstructions were
observed. However, the spongy showed some gingival lesions and bone
remnants between the dogs' teeth. Gingival lesions were caused by the
daily and continuous supply of new pieces of bone for the 13 days.
However, the bones failed to cure or even partially treat periodontal
disease, which is a below-the-gumline disorder. They stated:
"Although there was an improvement in the visual appearance of the gum, there was no reduction in plaque and calculus under the gumline. The maintenance of subgingival [below the gumline] plaque and calculus is the etiological factor of loss of dental adhesion to its alveolus, characteristic to periodontal disease. Thus, bones are not efficient in removing plaque and calculus under the gumline, they are only able to remove it on the crown."
February 2019:
Cat study finds 1-tetradecanol complex (1-TDC) applied to gums
significantly reduced periodontal disease.
 In a
February
2019 article by Brazilian dental specialists Fernanda Maria Lopes
Kubitza (right) and James Mudie George Anthony, they orally
applied the fatty acid combination of 1-tetradecanol complex (1-TDC) to
the teeth of nine cats (compared to the olive oil placebo to four other
cats) all of which had been diagnosed with moderate-to-severe
periodontal disease over a period of six weeks. Gel capsules of the
ingredients were squeezed into the cats' mouths once a day. The 1-TDC
capsules contained 525 mg each. At the end of the 6-week study, they
report finding "significant reductions in all parameters of clinical
periodontal disease", which included "clinical attachment level",
"gingival index", and "beeding on probing". There also was a decrease in
tooth mobility in the 1-TDC group cats, but it was not statistically
significant. They acknowledged that the "underlying mechanisms of action
of 1-TDC is still not elucidated". They concluded that daily 1-TDC
treatment of periodontal disease in cats should be considered to manage
In a
February
2019 article by Brazilian dental specialists Fernanda Maria Lopes
Kubitza (right) and James Mudie George Anthony, they orally
applied the fatty acid combination of 1-tetradecanol complex (1-TDC) to
the teeth of nine cats (compared to the olive oil placebo to four other
cats) all of which had been diagnosed with moderate-to-severe
periodontal disease over a period of six weeks. Gel capsules of the
ingredients were squeezed into the cats' mouths once a day. The 1-TDC
capsules contained 525 mg each. At the end of the 6-week study, they
report finding "significant reductions in all parameters of clinical
periodontal disease", which included "clinical attachment level",
"gingival index", and "beeding on probing". There also was a decrease in
tooth mobility in the 1-TDC group cats, but it was not statistically
significant. They acknowledged that the "underlying mechanisms of action
of 1-TDC is still not elucidated". They concluded that daily 1-TDC
treatment of periodontal disease in cats should be considered to manage the disorder.
the disorder.
EDITOR'S NOTE: We are including this report about cats because, thus far, we have found no similar studies including dogs. In one prior study of fifteen rabbits with experimentally induced periodontitis, 1-TDC had been found effective in reducing inflammation in the gums of the ten rabbits in the treatment groups.
June 2018:
Periodontal disease is suspected cause of bacterial
meningoencephalomyelitis in a cavalier.
 In
a
June 2018 article, a team of PennVet clinicians (Alexander E. Tun
[right], Leontine Benedicenti, Evelyn M. Galban) diagnosed
meningoencephalomyelitis caused by the bacteria Pasteurella multocida in
a 5-year-old cavalier King Charles spaniel. (Meningoencephalomyelitis
[MEM] is inflammation of the brain, including its protective membranes,
and of the spinal cord, caused by a bacteria.) The dog had severe
periodontal disease, with contact ulceration and possible necrotizing
stomatitis. Her symptoms included fever, lethargy, inappetence, and
multifocal neurologic signs, mainly dull mentation. Based upon
examination of her cerebrospinal fluid (CSF) and blood culture, and her
response to therapy (anti-emetics and gastroprotectants, an opioid for
analgesia, and dexamethasone sodium phosphate as an antiinflammatory),
P. multocida meningoencephalomyelitis was diagnosed. They opine that the
severe periodontal disease led to a bacteremia causing hematogenous
seeding of a bacterial meningitis originating at the disrupted
blood-spinal cord barrier.They concluded:
In
a
June 2018 article, a team of PennVet clinicians (Alexander E. Tun
[right], Leontine Benedicenti, Evelyn M. Galban) diagnosed
meningoencephalomyelitis caused by the bacteria Pasteurella multocida in
a 5-year-old cavalier King Charles spaniel. (Meningoencephalomyelitis
[MEM] is inflammation of the brain, including its protective membranes,
and of the spinal cord, caused by a bacteria.) The dog had severe
periodontal disease, with contact ulceration and possible necrotizing
stomatitis. Her symptoms included fever, lethargy, inappetence, and
multifocal neurologic signs, mainly dull mentation. Based upon
examination of her cerebrospinal fluid (CSF) and blood culture, and her
response to therapy (anti-emetics and gastroprotectants, an opioid for
analgesia, and dexamethasone sodium phosphate as an antiinflammatory),
P. multocida meningoencephalomyelitis was diagnosed. They opine that the
severe periodontal disease led to a bacteremia causing hematogenous
seeding of a bacterial meningitis originating at the disrupted
blood-spinal cord barrier.They concluded:
"In the future, be aware that a fever with multifocal neurologic signs and severe periodontal disease in a canine patient may suggest a P. multocida infection and both CSF and blood cultures can be submitted for confirmation."
April
2018:
Cavalier with severe periodontal disease develops Pasteurella
Multocida meningoencephalomyelitis.
 In an
April 2018 article, a team of University of Pennsylvania
neurologists (Alexander E. Tun [right], Leontine Benedicenti,
Evelyn M. Galban) report on a 5-year-old spayed female cavalier King
Charles spaniel with severe periodontal disease which had developed
Pasteurella Multocida meningo-encephalomyelitis causing signs of a
neurological disorder. Based on cerebrospinal fluid and blood culture,
as well as response to therapy, they opine that the severe periodontal
disease led to a bacteremia causing hematogenous seeding of a bacterial
meningitis originating at the disrupted blood-spinal cord barrier.
In an
April 2018 article, a team of University of Pennsylvania
neurologists (Alexander E. Tun [right], Leontine Benedicenti,
Evelyn M. Galban) report on a 5-year-old spayed female cavalier King
Charles spaniel with severe periodontal disease which had developed
Pasteurella Multocida meningo-encephalomyelitis causing signs of a
neurological disorder. Based on cerebrospinal fluid and blood culture,
as well as response to therapy, they opine that the severe periodontal
disease led to a bacteremia causing hematogenous seeding of a bacterial
meningitis originating at the disrupted blood-spinal cord barrier.
April 2015:
Dental disease was second to only heart murmurs in cavaliers in
the UK in a 6-year veterinary records review.
 In
an
April 2015 article, a team of UK veterinary researchers (Jennifer F.
Summers [right], Dan G. O'Neill, David B. Church, Peter C.
Thomson, Paul D. McGreevy, David C. Brodbelt) reviewed the primary-care
medical records of 1,875 cavalier King Charles spaniels from July 2007
to July 2013. They categorized the most common specific disorders
recorded by the examining veterinary clinicans, as follows: First were
heart murmurs, followed by dental disease, including periodontal
disorders. Dental disorders were included only when severe enough to
result in a veterinary recommendation for medical or surgical
intervention.
In
an
April 2015 article, a team of UK veterinary researchers (Jennifer F.
Summers [right], Dan G. O'Neill, David B. Church, Peter C.
Thomson, Paul D. McGreevy, David C. Brodbelt) reviewed the primary-care
medical records of 1,875 cavalier King Charles spaniels from July 2007
to July 2013. They categorized the most common specific disorders
recorded by the examining veterinary clinicans, as follows: First were
heart murmurs, followed by dental disease, including periodontal
disorders. Dental disorders were included only when severe enough to
result in a veterinary recommendation for medical or surgical
intervention.
RETURN TO TOP
Related Links
Veterinary Resources
Effect of Coenzyme Q10, on Experimental Periodontitis in Dogs. Satoshi Shizukuishi, Eiji Inoshita, Akira Tsunemitsu, Kyoko Nagae, Takeo Kishi, Karl Folkers. Biomed. Res. January 1983;4(1):33-40. Quote: Experimental periodontitis was induced in dogs by the use of cotton floss. The animals were divided into four groups. The control group of dogs (I) had their teeth cleaned with a toothbrush. The CoQ10-treated control group (II) also had their teeth cleaned with a toothbrush while Coenzyme Q10 (CoQ10) was administered daily for 2 weeks. In the periodontitis control group (III), the cotton floss ligatures were left around the teeth during the 28-day period. In the CoQ10-treated periodontitis group (IV), periodontitis resulted from the ligatures, and treatment with CoQ10-, was administered daily for 2 weeks. The scores of gingival index and pocket depth for group IV, which was treated with CoQ10, were significantly lower than in group III. No difference was found in these parameters for group I and II. These results indicate that the oral administration of CoQ10, is effective in suppressing advanced periodontal inflammation as assessed by gingival index and pocket depth. The CoQ10, levels in gingiva of group IV were significantly higher than in group II, but no diflerence was observed in the CoQ10, levels in plasma for group II and IV. These results show that the oral administration of CoQ", increases the CoQ10 levels in the gingiva of the dogs with periodontitis, but not in dogs with normal gingiva. The activity of the CoQ-dependent enzymes in group IV was significantly elevated in comparison with those of group III, and the CoQ- % deficiency of succinic cytochrome c reductase in group IV was restored to normal level.
Association of Periodontal Disease and Histologic Lesions in Multiple Organs from 45 Dogs. Linda J. DeBowes, Derek Mosier, Ellen Logan, Colin E. Harvey, Stephen Lowry, Daniel C. Richardson. J. Vet. Dent. June 1996;13(2):57-60. Quote: Forty-five mixed breed dogs were evaluated for the presence and extent of periodontal disease. Histopathobgy was performed on samples of lung, myocardium, liver, kidney, tonsil, spleen, submandibular lymph node and tracheobronchial lymph node. Mitral valves were evaluated grossly. Statistical analysis was used to determine if there was a relationship between the extent of periodontal disease and histopathologic changes in the tissues examined. In the forty-five dogs studied, an association was found between periodontal disease and histopathologic changes in kidney, myocardium (papillary muscle), and liver.
Periodontal Disease in Dogs: Etiopathogenesis, Prevalence, and Significance. Colin E. Harvey. Vet. Clinics: Sm. Anim. Pract. September 1998; doi: 10.1016/S0195-5616(98)50105-2. Quote: Periodontal disease is probably the most common disease in dogs; however, clinical periodontal disease seems to be an uncommon cause of severe illness. Why then should we be concerned with something that is apparently compatible with life most of the time, even if it is so common? This article answers this question. To do so, the disease process and prevalence must be considered, so that this and additional information in other articles in this issue (e.g., the article by DuPont) can put into perspective the significance of periodontal disease in dogs.
Effect of a mucoadhesive gel and dental scaling on gingivitis in dogs. D Bonello, P Squarzoni. J. Vet. Dent. March 2008; doi: 10.1177/089875640802500108. Quote: Twenty client-owned dogs diagnosed with gingivitis were studied over a 45-day period in order to investigate the effect of professional dental prophylaxis combined with the use of a topical mucoadhesive gel containing adelmidrol, an aliamide. A non-intrusive papillary-marginal-gingival index (PMGI) was measured at each assessment, while the gingivitis index (GI) was measured only at the beginning and end of the study. Compared to the control group, the treated dogs had a significant decrease (P < 0.005) in the average GI index during the course of the study. A significant reduction (P < 0.002) in the average PMGI index was observed in both groups 15-days following dental prophylaxis. However at 30 and 45-days following dental prophylaxis, the PMGI index values were significantly different (P < 0.005) from baseline only in treated dogs. These results suggest that the combined use of a mucoadhesive gel with dental scaling was able to improve the regression of gingival inflammation and lengthen the therapeutic benefits of dental scaling and polishing during a limited study period.
Periodontal Disease. Brook A. Niemiec. Topics in Companion Anim. Med. May 2008;23(2):72-80. Quote: Periodontal disease is the most commonly diagnosed problem in small animal veterinary medicine. In the vast majority of cases, however, there are little to no outward clinical signs of the disease process, and, therefore, therapy often comes very late in the disease course. Consequently, periodontal disease is also the most undertreated animal health problem. In addition, unchecked periodontal disease has numerous dire consequences both locally and systemically. These consequences are detailed in the article and should be utilized to educate clients and encourage compliance of therapeutic recommendations. The local consequences include oronasal fistulas, class II perio-endo lesions, pathologic fractures, ocular problems, osteomyelitis, and an increased incidence of oral cancer. Systemic diseases linked to periodontal disease include: renal, hepatic, pulmonary, and cardiac diseases; osteoporosis, adverse pregnancy effects, and diabetes mellitus. Before the discussion of consequences, this article covers the pathogenesis of periodontal disease, followed by clinical features and diagnostic tests.
Malocclusion associated with macroglossia in a dog. Gerhard Putter. UK Vet. Companion Anim. November 2011; doi:10.1111/j.2044-3862.2011.00108.x. Quote: Macroglossia (defined as enlargement of the tongue but not indicating the cause) is a rare condition in dogs. The association with malocclusion has not been described before. It has been reported that resection of as much as 60% of the body of the tongue is well tolerated by dogs. Although the tongue is a very vascular organ, intraoperative haemorrhage during tongue amputation can be effectively controlled by a tourniquet at the base of the tongue. Healing of the amputation wound is usually rapid and uneventful. ... A five year old, 12 kg neutered male Cavalier King Charles Spaniel was presented with a complaint of an excessively long tongue. ... During panting, the dog's tongue protruded about 10 cm from the left side of the mouth (Fig. 1). Any attempt by the dog to withdraw the tongue into the mouth caused the left upper lip to be drawn into the mouth. It was therefore not possible for the dog to return the tongue to its normal intraoral position. This caused the surface of the left upper lip to be constantly wet with saliva. ... Generalised moderate calculus associated with slight to moderate gingivitis was present. ... The pressure from the deviated tongue on the left maxillary as well as mandibular premolars has caused the deviation of these teeth laterally. This also explains the greater rotation and deviation of the rostral aspect of the left mandible because more pressure was exerted by the tongue on these teeth. At some stage during the progression of the condition, the left upper lip has become involved. The hair on the upper lip appears to have prevented complete retraction of the tongue into the mouth and to have caused the lip to be drawn into the left side of the oral cavity. ... The owner opted not to consider surgical repair of the malocclusion and the deviation of the left mandible. Surgery to reduce the length of the tongue was scheduled for a later date that suited the owner. ... Resection of 40-60% of the rostral aspect of the tongue is well tolerated by most dogs and cats. This case was no exception and an even larger segment could have been resected.
A case-control study between interleukin-10 gene variants and periodontal disease in dogs. Carlos Albuquerque, Francisco Morinha, João Requicha, Isabel Dias, Henrique Guedes-Pinto, Carlos Viegas, Estela Bastos. Gene. April 2014;539(1):75-81. Quote: "Periodontal disease (PD) refers to a group of inflammatory diseases caused by bacterial plaque in the periodontium and ranges from an early stage (gingivitis) to an advanced stage (periodontitis). It is a multifactorial disease that results from the interaction of the host defence mechanisms with the plaque microorganisms. PD has an enormous impact on human medicine and veterinary medicine due to its high prevalence as well as its local and systemic implications. Dog model has been extensively used in oral disease research, contributing significantly to the current understanding of periodontology. The most important clinical aspects of canine PD were considered in this work and the various animal models were examined with emphasis on the role of the dog as the most useful model for understanding human PD and to develop new therapeutic and preventive measures. In recent decades, it has been consolidated the idea of the genetics influence in PD by controlling the inflammatory process severity and the therapy responses. Various single nucleotide polymorphisms have been identified as risk factors, mainly in genes responsible for molecules involved in immunoregulation and/or metabolism, but many questions still remain. In canine PD, this is a completely unexplored issue but a highly relevant and promising research field namely because the strong similarity between canine and human disease provides the possibility to share the knowledge attained from one species to another, with mutual benefits. Following a comparative genomics approach to identify the most promising candidate genes, the main goal of this work was to contribute for a better characterization of canine PD, particularly in terms of genetic basis. Five candidate genes (IL1A, IL1B, IL10, IL6 and LTF) encoding molecules with recognized relevant role in the PD pathogenesis (interleukin-1a, interleukin-1B, interleukin-10, interleukin-6 and lactotransferrin, respectively) were selected and case-control studies were delineated, in which a molecular analysis of each gene was performed to identify genetic variations and to evaluate its possible association with PD. It was hypothesized that in canine PD, similar to human PD, a disfunction or a dysregulated production of these molecules resulting from genetic variations can be part of the explanation for the differences in disease susceptibility between individuals. A total of twenty-six genetic variations were identified and analyzed, eight in the IL1A and IL1B genes, seven in the IL10 gene, three in the IL6 gene, and eight in the LTF gene. The IL1A/1_g.388A>C and IL1A/1_g.521T>A variations showed statistically significant differences between groups [adjusted OR (95%CI): 0.15 (0.03-0.76), p=0.022; 5.76 (1.03-32.1), p=0.046, respectively], meaning that, in the studied population, the IL1A/1_g.388C allele is associated with a decreased PD risk, whereas the IL1A/1_g.521A allele is associated with an increased risk. Regarding all the others variations, no statistically significant differences were detected, but the IL1A/2_g.515G>T, IL10/2_g.285G>A, IL6/2_g.105G>A, LTF/3_g.411C>T, LTF/3_g.420G>A and LTF/3_g.482G>A variations resulted in a change of encoded amino acid, which may alter protein structure and function, as demonstrated by different bioinformatics tools. Before the molecular analysis of the IL10 gene, two additional studies were delineated. Considering that no clear consensus has been reached about the association of IL10 polymorphisms and human PD, a meta-analysis of all available studies was performed. It was found statistically significant association of IL10-819(-824)C>T and IL10-592(-597)C>A polymorphisms, with IL10-819(-824)T and -592(-597)A alleles conferring a relative increased risk for chronic periodontits in Caucasians. Additionally, a study to evaluate the levels of interleukin-10 in plasma of dogs with periodontitis was delineated assessing a possible correlation between these levels and periodontal condition, being found lower levels in the periodontitis group comparing with the control group. The outcome from this work suggests that dog IL1A, IL1B, IL10, IL6 and LTF genes, as occurs in the human orthologous genes, are highly polymorphic with genetic variants that may be important in PD susceptibility. ... Short et al. (2007) developed an analysis of candidate susceptibility genes in canine diabetes, including IL10 gene, selected taking in account the previous associations described in human diabetes. These authors found various polymorphisms in dog IL10 gene associated with diabetes mellitus in the Cavalier King Charles Spaniel. ... The results obtained for the IL1A are particularly relevant, but this is the first work in this issue and further studies are essential to reinforce these findings and to clarify its biological importance; as well as other studies with different candidate genes. But, it is undeniable that advances in this area are fundamental to understand properly the complex causal pathways of PD and to improve the clinical management of PD, particularly with the development of novel strategies of risk assessment. A candidate gene approach supported in comparative genomics tools is a promising path of research to achieve these objectives, which may lead to great benefits in human and veterinary periodontology, adding important knowledge to design new preventive and therapeutic strategies, and ultimately to improve health in both humans and dogs.
Prevalence of disorders recorded in Cavalier King Charles Spaniels attending primary-care veterinary practices in England. Jennifer F. Summers, Dan G. O'Neill, David B. Church, Peter C. Thomson, Paul D. McGreevy, David C. Brodbelt. Canine Genetics & Epidemiology. April 2015; doi: 10.1186/s40575-015-0016-7. Quote: Background: Concerns have been raised over breed-related health issues in purebred dogs, but reliable prevalence estimates for disorders within specific breeds are sparse. Electronically stored patient health records from primary-care practice are emerging as a useful source of epidemiological data in companion animals. This study used large volumes of health data from UK primary-care practices participating in the VetCompass animal health surveillance project to evaluate in detail the disorders diagnosed in a random selection of over 50% of dogs recorded as Cavalier King Charles Spaniels (CKCSs). Confirmation of breed using available microchip and Kennel Club (KC) registration data was attempted. Results: In total, 3624 dogs were recorded as CKCSs within the VetCompass database of which 143 (3.9%) were confirmed as KC-registered via microchip identification linkage of VetCompass to the KC database. 1875 dogs (75 KC registered and 1800 of unknown KC status, 52% of both groups) were randomly sampled for detailed clinical review. Clinical data associated with veterinary care were recorded in 1749 (93.3%) of these dogs. The most common specific disorders recorded during the study period were heart murmur (541 dogs, representing 30.9% of study group), diarrhoea of unspecified cause (193 dogs, 11.0%), dental disease (166 dogs, 9.5%), otitis externa (161, 9.2%), conjunctivitis (131, 7.4%) and anal sac infection (129, 7.4%). The five most common disorder categories were cardiac (affecting 31.7% of dogs), dermatological (22.2%), ocular (20.6%), gastrointestinal (19.3%) and dental/periodontal disorders (15.2%). Discussion and conclusions: Study findings suggest that many of the disorders commonly affecting CKCSs are largely similar to those affecting the general dog population presented for primary veterinary care in the UK. However, cardiac disease (and MVD in particular) continues to be of particular concern in this breed. ... Dental disorders were included only when severe enough to result in a veterinary recommendation for medical or surgical intervention. ... Further work: This work highlights the value of veterinary practice based breed-specific epidemiological studies to provide targeted and evidence-based health policies. Further studies using electronic patient records in other breeds could highlight their potential disease predispositions.
Tooth brushing inhibits oral bacteria in dogs. Kazuhiro Watanabe, Kotaro Hayashi, Saku Kijima, Chie Nonaka, Kazuaki Yamazoe. J. Vet. Med. Sci. May 2015; doi: 10.1292/jvms.14-0193. Quote: In this study, scaling, polishing and daily tooth brushing were performed in 20 beagle dogs, and the number of oral bacteria was determined using a bacterial counter. The dogs were randomized into the scaling (S), scaling + polishing (SP), scaling + tooth daily brushing (SB) and scaling + polishing + tooth daily brushing (SPB) groups. Samples were collected from the buccal surface of the maxillary fourth premolars of the dogs immediately after scaling and every week thereafter from weeks 1 to 8. Throughout the study, the number of bacteria was significantly lower in the SB and SPB groups compared with the S group. The findings suggest that daily tooth brushing inhibited oral bacterial growth in the dogs.
Raw beef bones as chewing items to reduce dental calculus in Beagle dogs. F R Marx, G S Machado, J G Pezzali, C S Marcolla, A M Kessler, Ø Ahlstrøm, L Trevizan. Aust. Vet. J. January 2016; doi: 10.1111/avj.12394. Quote: Objective: Evaluate the effect of raw bovine cortical bone (CB) (medullary bone cross-sectioned) and marrow or epiphyseal 'spongy' bone (SB) as chew items to reduce dental calculus in adult dogs. Methods: Eight 3-year-old Beagle dogs were observed in two study periods. In the first study, the dogs each received a piece of bovine femur CB (122 ± 17 g) daily and in the second study, a piece of bovine femur SB (235 ± 27 g). The first study lasted 12 days and the second 20 days. Dental calculus was evaluated using image integration software. Results: At the start of the studies, dental calculus covered 42.0% and 38.6% of the dental arcade areas, respectively. In study one, the chewing reduced the established dental calculus area to 27.1% (35.5% reduction) after 3 days and after 12 days the dental calculus covering was reduced to 12.3% (70.6% reduction). In study two, the dental calculus covered 16.8% (56.5% reduction) after 3 days, 7.1% (81.6% reduction) after 12 days and 4.7% (87.8% reduction) after 20 days. The CB remained largely intact after 24 h, but SB was reduced to smaller pieces and in some cases totally consumed after 24 h. No complications such as tooth fractures, pieces of bone stuck between teeth or intestinal obstructions were observed during the studies. Conclusions: Chewing raw bovine bones was an effective method of removing dental calculus in dogs. The SB bones removed dental calculus more efficiently in the short term.
Inhibitory effect for proliferation of oral bacteria in dogs by tooth brushing and application of toothpaste. Kazuhiro Watanabe, Saku Kijima, Chie Nonaka, Yuki Matsukawa, Kazuaki Yamazoe. J. Vet. Med. Sci. April 2016; doi: 10.1292/jvms.15-0277. Quote: To investigate inhibitory effect for oral bacterial proliferation, we divided 12 dogs into 3 groups; scaling alone (C; control group), brushing (B) and application of toothpaste (P). Before scaling (Pre) and at 0 to 8 weeks after scaling (0-8 w), we collected oral bacteria from the dental surface every week and counted them using a bacterial counter. The results demonstrated a significant reduction in the number of oral bacteria for group B relative to Pre and group C, as well as for group P relative to group C at 5-7 w. Consequently, brushing may inhibit an increase in the number of oral bacteria, and toothpaste may be effective at a certain level, although not more than that of brushing.
The genetics of canine periodontal disease -- A candidate gene approach. Carlos Manuel Ramos Albuquerque. Thesis, Universidade de Trás-os-Montes e Alto Douro. 2017. Quote: Periodontal disease (PD) refers to a group of inflammatory diseases caused by bacterial plaque in the periodontium and ranges from an early stage (gingivitis) to an advanced stage (periodontitis). It is a multifactorial disease that results from the interaction of the host defence mechanisms with the plaque microorganisms. PD has an enormous impact on human medicine and veterinary medicine due to its high prevalence as well as its local and systemic implications. Dog model has been extensively used in oral disease research, contributing significantly to the current understanding of periodontology. The most important clinical aspects of canine PD were considered in this work and the various animal models were examined with emphasis on the role of the dog as the most useful model for understanding human PD and to develop new therapeutic and preventive measures.
Oscar's Braces. San Juan Veterinaary Clinic. March 2018. Oscar is the world's sweetest 8-month-old, neutered male Cavalier King Charles Spaniel. He was presented to us because the owner noticed his baby teeth did not fall out like they should have. ... Oscar has failed to shed his deciduous k9 teeth. Under normal circumstances, the root of the tooth is resorbed, and the crown is exfoliated, then the adult tooth erupts into its place. If this process fails, the baby tooth remains in place leaving the adult tooth no place to go as it erupts. As a result, the adult tooth is displaced into an abnormal position. In this case (which is typical of nearly all cases) the adult k9 tooth has been displaced forward. Oscar now has 2 major dental problems: 1) His adult k9 teeth are interfering (hitting each other) causing significant tooth wear and pressure and causing his mandible to be pushed to the left when he closes his mouth. Because of this, when Oscar closes his mouth his lower right k9 tooth has to rest to the inside of the top right k9 tooth. This is causing a traumatic pocket in the soft tissue of his palate which is painful. ... The entire root of the baby tooth is still present which is why the tooth didn't fall out. The 2nd problem that Oscar now has is the certain rapid development of periodontal disease due to the crowding of the baby tooth and adult tooth. For these reasons, we very delicately and surgically removed the entire baby tooth and decided to use active orthodontic force to move the adult tooth back into its normal position.
Pasteurella Multocida meningoencephalomyelitis in a dog secondary to severe periodontal disease. Alexander E. Tun, Leontine Benedicenti, Evelyn M. Galban. Clin. Case. Repts. June 2018; doi: 10.1002/ccr3.1561. Quote: Pasteurella multocida can cause meningoencephalomyelitis in canine patients with severe periodontal disease. Fever and neutrophilic pleocytosis in the cerebrospinal fluid are likely, and blood culture and/or empiric antibiotic therapy are indicated. ... A 5-year-old 5.14 kg (11.3-lb) spayed female Cavalier King Charles Spaniel was presented to the Neurology and Neurosurgery service at the Matthew J. Ryan Veterinary Hospital of the University of Pennsylvania for evaluation of ataxia and cervical hyperesthesia. The day prior the patient was initially presented to the referring veterinarian for a 2‐day history of lethargy and inappetence. ... Consultation by the Dentistry and Oral Surgery Service confirmed the severe periodontal disease with contact ulceration and possible necrotizing stomatitis. However, the changes were not considered to be to the degree that would cause lethargy and inappetence, and so dental cleaning with extractions was recommended once the patient condition had stabilized. ... As the patient described had no such inoculation or injury, it is the hypothesis of the authors that this patient's severe periodontal disease leads to a bacteremia causing hematogenous seeding of a bacterial meningitis originating at the disrupted blood-spinal cord barrier. ... The patient described exhibited clinical signs and laboratory findings consistent with previous reports of bacterial MEM [meningoencephalomyelitis] in dogs. Based on CSF and blood culture, as well as response to therapy, a diagnosis of P. multocida meningoencephalomyelitis was made. This is the first report of a canine patient with a P. multocida CNS infection without evidence of a direct inoculation. In addition, this is the first report where the source of the infection is suspected to be severe periodontal disease. Further support for this theory might have come from concurrent culture of the oral flora or any extracted teeth with matching susceptibility pattern. In the future, be aware that a fever with multifocal neurologic signs and severe periodontal disease in a canine patient may suggest a P. multocida infection and both CSF and blood cultures can be submitted for confirmation.
Topical oral 1-tetradecanol complex in the treatment of periodontal diseases in cats. Fernanda Maria Lopes Kubitza, James Mudie George Anthony. J. Feline Med. & Surg. February 2019; doi: 10.1177/1098612X18820734. Quote: Objectives: The aim of this study was to evaluate the outcomes of the treatment of chronic periodontal disease with an oral application of tetradecanol complex (1-TDC) in cats. Methods: The test group (n = 9) received 1-TDC (525 mg per gel capsule/day) and the placebo group (n = 4) received olive oil (0.25 ml per gel capsule/day) for 6 weeks. Results: Oral treatment with 1-TDC resulted in significant reductions in all parameters of clinical periodontal disease except tooth mobility at 6 weeks. The 1-TDC group exhibited a statistically significant reduction in pocket depth, clinical attachment loss, gingival index and bleeding on probing after treatment at 6 weeks, whereas the placebo group did not show any significant change. Conclusions and relevance: Chronic inflammation associated with periodontal diseases leads to periodontal tissue destruction. As a result, modulation of the host response has been included in the treatment protocol for periodontal diseases. Fatty acids present anti-inflammatory properties and are being investigated for use in the treatment and prevention of progressive periodontal diseases.
Evaluation of teeth injuries in Beagle dogs caused by autoclaved beef bones used as a chewing item to remove dental calculus. Caroline Fredrich Dourado Pinto, Willian Lehr, Víviam Nunes Pignone, Caio Peixoto Chain, Luciano Trevizan. PLos ONE. February 2020; doi: 10.1371/journal.pone.0228146. Quote: Dental calculus (DC) is the most widespread oral problem in domestic dogs. Chewing items are used to remove DC from the tooth surface; they also favor oral health and animal welfare. Raw beef bone mastication also shortly reduces DC in adult dogs. However, it can cause oral lesions and hence is not popular. This study evaluated the impact of bone mastication on the dental roots, enamel, and gingiva of dogs. Twelve adult Beagle dogs were randomly divided into 2 treatment groups in a completely randomized block design: cortical bone (CB) or spongy bone (SB). Intraoral radiographs were obtained on days 0 and 14, and calculus assessment was performed using images captured on days 0, 3, 6, 9, 12, and 14; an integration program was used to measure the proportion between the area covered by calculus and the total area of teeth. DC was completely removed from the first and second premolars and molars from both the arcades in less than 3 days of supplementation, indicating that these teeth were frequently used for chewing (P < 0.10). Bones were highly effective for DC removal and gingival inflammation reduction. Despite the hardness of bones, no lesions or teeth root and enamel fracture, or esophageal or intestinal obstructions--complications related to bone ingestion--were noted. However, SB showed some gingival lesions (n = 4) and bone remnants between teeth (n = 2). Gingival lesions were caused by the daily and continuous supply of new pieces of bone for 13 days. Specific pieces of bone should be used for oral home care programs because they shortly remove almost 90% of DC, allowing longer intervals between periodontal cleaning procedures. ... Although there was an improvement in the visual appearance of the gum, there was no reduction in plaque and calculus under the gumline. The maintenance of subgingival plaque and calculus is the etiological factor of loss of dental adhesion to its alveolus, characteristic to periodontal disease. Thus, bones are not efficient in removing plaque and calculus under the gumline, they are only able to remove it on the crown. ... Long-term studies are required to evaluate the use of bones and evaluate their impact on teeth and periodontium after prolonged supplementation.
World Small Animal Veterinary Association Global Dental Guidelines. B. Niemiec, J. Gawor, A. Nemec, D. Clarke, K. McLeod, C. Tutt, M. Gioso, P. V. Steagall, M. Chandler, G. Morgenegg, R. Jouppi. J. Sm. Anim. Pract. July 2020;61:E36-E161. Quote: Dental, oral, and maxillofacial diseases are some of the most common problems in small animal veterinary practice. These conditions create significant pain as well as localized and potentially systemic infection. As such, the World Small Animal Veterinary Association (WSAVA) believes that un- and under treated oral and dental diseases pose a significant animal welfare concern. Dentistry is an area of veterinary medicine which is still widely ignored and is subject to many myths and misconceptions. Effective teaching of veterinary dentistry in the veterinary school is the key to progression in this field of veterinary medicine, and to the improvement of welfare for all our patients globally. These guidelines were developed to provide veterinarians with the information required to understand best practices for dental therapy and create realistic minimum standards of care. Using the three-tiered continuing education system of WSAVA, the guidelines make global equipment and therapeutic recommendations and highlight the anaesthetic and welfare requirements for small animal patients. This document contains information on common oral and dental pathologies, diagnostic procedures (an easily implementable and repeatable scoring system for dental health, dental radiography and radiology) and treatments (periodontal therapy, extractions). Further, there are sections on anaesthesia and pain management for dental procedures, home dental care, nutritional information, and recommendations on the role of the universities in improving veterinary dentistry. A discussion of the deleterious effects of anaesthesia free dentistry (AFD) is included, as this procedure is ineffective at best and damaging at worst. Throughout the document the negative effects of undiagnosed and/or treated dental disease on the health and well-being of our patients, and how this equates to an animal welfare issue, is discussed.
Prevalence of commonly diagnosed disorders in UK dogs under primary veterinary care: results and applications. Dan G. O'Neill, Hannah James, Dave C. Brodbelt, David B. Church, Camilla Pegram. BMC Vet. Res. February 2021; doi: 10.1186/s12917-021-02775-3. Quote: Background: Although dogs are a commonly owned companion animal in the UK, the species experiences many health problems that are predictable from demographic information. This study aimed to use anonymised veterinary clinical data from the VetCompass™ Programme to report the frequency of common disorders of dogs under primary veterinary care in the UK during 2016 and to explore effects associated with age, sex and neuter status. Results: From an available population of 905,543 dogs under veterinary care at 886 veterinary clinics during 2016, the current study included a random sample of 22,333 (2.47 %) dogs from 784 clinics. Prevalence for each disorder was calculated at the most refined level of diagnostic certainty (precise-level precision) and after grouping to a more general level of diagnostic precision (grouped-level precision). The most prevalent precise-level precision disorders recorded were periodontal disease (prevalence 12.52%, 95% CI: 12.09-12.97), otitis externa (7.30%, 95% CI: 6.97-7.65) and obesity (7.07%, 95% CI: 6.74-7.42). The most prevalent grouped-level disorders were dental disorder (14.10%, 95% CI: 13.64-14.56), skin disorder (12.58%, 95% CI: 12.15-13.02) and enteropathy (10.43%, 95% CI: 10.04-10.84). Associations were identified for many common disorders with age, sex and neuter. Conclusions: The overall findings can assist veterinarians and owners to prioritise preventive care and to understand demographic risk factors in order to facilitate earlier diagnosis of common disorders in dogs. The information on associations with age, sex and neuter status provides additional contextual background to the complexity of disorder occurrence and supports targeted health controls for demographic subsets of dogs.
Periodontal disease is associated with cognitive dysfunction in aging dogs: A blinded prospective comparison of visual periodontal and cognitive questionnaire scores. Curtis Wells Dewey, Mark Rishniw. Open Vet. J. April 2021; doi: 10.5455/OVJ.2021.v11.i2.4. Quote: Background: Periodontal disease has been linked to the development of Alzheimer's disease in people. It is theorized that the chronic inflammatory condition characteristic of oral dysbiosis in patients with periodontal disease leads to disruption of the blood-brain barrier, cytotoxin- and pathogen-induced brain damage, and accumulation of neurotoxic B-amyloid. In this inflammatory theory of Alzheimer's disease, B-amyloid--a known antimicrobial protein-- accumulates in response to oral pathogens. Canine cognitive dysfunction (CCD) is considered a naturally occurring animal model of human Alzheimer's disease. Like humans, periodontal disease is quite common in dogs; however, a link between periodontal disease and cognitive dysfunction has not been identified in this species. Aim: The purpose of this prospective investigation was to compare visual periodontal scores (from digital oral photographs) with numerical (0-54) cognitive assessment questionnaire forms in aging dogs with and without a clinical diagnosis of CCD. Methods: A visual analogue scale (0-4) was used to score the severity of periodontal disease in 21 aging dogs: 11 dogs with a clinical diagnosis of presumptive CCD and 10 dogs [including one cavalier King Charles spaniel] without a clinical history of cognitive decline. Individuals scoring the dental photographs were blinded to all case information, including cognitive assessment scores. Cognitive assessment scores were compared with periodontal disease scores for all dogs. Results: There was a significant association between periodontal and cognitive scores, with higher cognitive impairment scores being more likely in dogs with more severe periodontal disease and vice versa. No associations were identified between age and either periodontal disease or cognitive impairment. Conclusion: ... Our study is the first to identify an association between visually categorized periodontal disease and CCD. ... Although a cause-and-effect relationship between periodontal disease and cognitive impairment cannot be ascertained from this preliminary study, we established a link between these two disorders that warrants further investigation using more stringent criteria for evaluating both periodontal disease and cognitive dysfunction.
Breed Predispositions to Dental and Oral Disease in Dogs. Brook Niemiec, editor. John Wiley & Sons. March 2021; doi: 10.1002/9781119552031
Conditions Common in Small and Toy Breed Dogs. Brook A.
Niemiec. Chapter 1 in: Breed Predispositions to Dental and Oral Disease
in Dogs. Brook Niemiec, editor. John Wiley & Sons. March 2021;
ISBN: 978-1-119-55204-8. Quote: The
major difference between at risk (small breed dogs as well as greyhounds
and Cavalier King Charles Spaniels [CKCS]) and
traditional dogs is the frequency of and age at initiation of
periodontal care. ... Brachycephalic Breeds and Periodontal Disease: In
general, these breeds do not appear to be more susceptible to
periodontal disease than others of their size
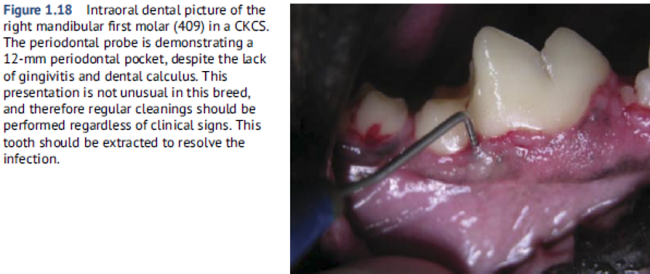 (with the exception of
Cavalier King Charles Spaniels). ... Cavalier
King Charles Spaniels (CKCS) and Greyhounds are well known for
significant periodontal disease. CKCS suffer from early
onset periodontal disease, especially in the maxillary premolars (as
they are similar to other brachycephalic breeds). There is quite often
furcation exposure of these teeth as early as two years of age.
Interestingly, it is quite common for them to have advance periodontal
loss with minimum calculus and gingivitis. (Figure 1.18). ... Both of these breeds are
very difficult to manage due to the high genetic potential for the
disease. They typically suffer from significant gingivitis and early
bone loss with only minimal calculus.
(with the exception of
Cavalier King Charles Spaniels). ... Cavalier
King Charles Spaniels (CKCS) and Greyhounds are well known for
significant periodontal disease. CKCS suffer from early
onset periodontal disease, especially in the maxillary premolars (as
they are similar to other brachycephalic breeds). There is quite often
furcation exposure of these teeth as early as two years of age.
Interestingly, it is quite common for them to have advance periodontal
loss with minimum calculus and gingivitis. (Figure 1.18). ... Both of these breeds are
very difficult to manage due to the high genetic potential for the
disease. They typically suffer from significant gingivitis and early
bone loss with only minimal calculus.
Influence of Dietary Supplementation With a Powder Containing A.N. ProDen™ (Ascophyllum Nodosum) Algae on Dog Saliva Metabolome. Jerzy Pawel Gawor, Jacek Wilczak, Ulla K. Svensson, Michal Jank. Front. Vet. Sci. June 2021; doi: 10.3389/fvets.2021.681951. Quote: The objective of this placebo-controlled, double-blind, randomized study (designed according to evidence-based medicine standards) was to determine the effect of 30-day administration of powdered brown algae, Ascophyllum nodosum (ProDen PlaqueOff, SwedenCare AB, Sweden), on saliva metabolomes in dogs. Sixty client-owned dogs underwent professional dental cleaning and were randomly subdivided into two groups receiving daily powdered brown algae A. nodosum, or a placebo (microcrystalline cellulose in powder), adjusted to their bodyweight. After a comprehensive oral health assessment and professional dental cleaning, which were both performed under general anesthesia, clinical assessments for gingivitis, plaque, and calculus were conducted. Saliva samples were collected at Day 0 and Day 30 of supplementation. Whole saliva is a mixed fluid that is derived predominantly from the major salivary glands but it also contains numerous other constituents. Additionally, its composition varies on whether salivary secretion is basal or stimulated. Authors put efforts to avoid contamination of saliva by other constituents and character of saliva was basal. Quadrupole time-of-flight (QTOF) mass spectrometer was used to conduct analysis of the saliva samples. Metabolomic analyses identified clear changes after 30 days of supplementation, and the direction of these changes was completely different than in dogs that received a placebo treatment during the same period. The positive clinical effect of 30 days of A. nodosum supplementation on oral health status in dogs described in previous publication combined with the absence of some metabolites in the saliva of dogs on day 30 of supplementation suggest that brown algae inhibit or turn off some pathways that could enhance plaque or calculus development. The exact mechanism of A. nodosum is still unclear and warrants further study.
Association of periodontal disease with breed size, breed, weight, and age in pure-bred client-owned dogs in the United States. Corrin Wallis, E.K. Saito, C. Salt, L.J. Holcombe, N.G. Desforges. Vet. J. July 2021; doi: 10.1016/j.tvjl.2021.105717. Quote: Despite periodontal disease (PD) being amongst the most common diagnoses in primary-care practice, the disease is generally underdiagnosed. ... Over 3 million medical records across 60 breeds of dogs visiting a chain [Banfield] of veterinary hospitals in the United States collected over a 5-year period were analysed. ... The 10 breeds with the highest prevalence of PD (Grades 1-4 combined) were: Greyhound (38.7%), Shetland sheepdog (30.6%), Papillon (29.7%), Toy poodle (28.9%), Miniature poodle (28.2%), Dachshund (28.1%), Bichon frise (27.9%), Cavalier King Charles spaniel (27.3%), American Eskimo dog (27.0%), Cairn terrier (26.8%). ... Cavalier King Charles spaniel had the highest probability of PD within the medium-small size category. ... The odds of a Cavalier King Charles spaniel having PD was 8.09 that of a French bulldog. ... Additional risk factors for PD diagnosis included age, being overweight and time since last scale and polish. Veterinarians should consider targeting client education about dental health, and diagnostic efforts, towards canine patients of the small-breed size categories and those with a higher risk of developing PD (e.g. overweight).
Epidemiology of periodontal disease in dogs in the UK primary-care veterinary setting. D. G. O'Neill, C. E. Mitchell, J. Humphrey, D. B. Church, D. C. Brodbelt, C. Pegram. J. Sm. Anim. Pract. August 2021; doi: 10.1111/jsap.13405. Quote: Objectives: Periodontal disease is a frequent diagnosis of dogs and can have severe negative impacts on welfare. It was hypothesised that breeds with skull shapes that differ most in conformation from the moderate mesocephalic skull shape have higher odds of periodontal disease. Materials and Methods: The cohort study included a random sample of dogs under primary veterinary care in 2016 from the VetCompass Programme database. Risk factor analysis used random effects multivariable logistic regression modelling. Results: ... The study included a random sample of 22,333 dogs attending 784 veterinary clinics from an overall population of 905,554 dogs under veterinary care in 2016. ... The 1-year period prevalence for diagnosis with periodontal disease was 12.52% (95% CI: 12.09 to 12.97). ... The breeds with the highest periodontal disease prevalence were Greyhound (32.21%), King Charles Spaniel (30.14%), Toy Poodle (25.97%), Cavalier King Charles Spaniel (25.29%), Yorkshire Terrier (22.22%) and Border Terrier (22.09%). ... Eighteen breeds showed increased odds compared with crossbred dogs. Breeds with the highest odds included Toy Poodle (odds ratio 3.97), King Charles Spaniel (odds ratio 2.63), Greyhound (odds ratio 2.58) and Cavalier King Charles Spaniel (odds ratio 2.39). Four breeds showed reduced odds compared with crossbreds. Brachycephalic breeds had 1.25 times the odds of periodontal disease compared with mesocephalic breeds. Spaniel types had 1.63 times the odds compared with non-spaniel types. Increasing adult bodyweight was associated with progressively decreasing odds of periodontal disease. ... Periodontal disease is shown to be a common diagnosis in UK dogs, with one in eight dogs diagnosed annually. There are strong breed predispositions for periodontal disease, with Toy Poodle, Greyhound and Cavalier King Charles Spaniel at greatest risk while German Shepherd Dog, French Bulldog and Staffordshire Bull Terrier showed reduced risk. ... Clinical Significance: The high prevalence identified in this study highlights periodontal disease as a priority welfare concern for predisposed breeds. Veterinarians can use this information to promote improved dental care in predisposed dogs, especially as these dogs age.
Evaluation of the Efficacy of Coenzyme Q10 in the Management of Chronic Periodontitis: A Clinical Study. Gaurav Pandav, Sakshi Pandav, Sanjeev Jain, Divya Saxena, Ridhi Aggarwal, Prerna Gulati. Dent. J. Adv. Stud. October 2021; doi:10.1055/s-0041-1736267. Quote: Aim: The present study was aimed to clinically evaluate the effectiveness of coenzyme Q10 (CoQ10) in the management of chronic periodontitis. Materials and Methods: A total of 60 [human] patients aged between 30 and 60 years with bleeding on probing and probing pocket depth (PPD) of 3 to 5 mm were selected and divided into three groups, with group I receiving scaling and root planing, group II CoQ10 formulation for 6 weeks, and group III receiving both scaling and root planning, followed by coenzyme Q10 administration for 6 weeks. PPD, relative attachment level (RAL), and gingival index were recorded in all the groups at baseline, 6 weeks, and 3 months, respectively. The data was statistically analyzed using Kruskal-Wallis, Mann-Whitney, and Wilcoxon signed rank tests. Result: Intragroup comparison showed statistically significant difference (p ≤ 0.05) between the clinical parameters of all the groups at all time intervals, whereas intergroup comparison of all the parameters showed high statistically significant difference (p ≤ 0.001) in group III at various time intervals followed by group I and group II. Conclusion: It was concluded from the study that CoQ10 is a useful adjunct in treating chronic periodontitis by boosting the host resistance to periodontal disease.
Prevalence of Dental and Skeletal Malocclusions in Mesaticephalic and Dolichocephalic Dogs -- a Retrospective Study (2015-2018). Marissa Berman, Maria Soltero-Rivera, Amy J Fulton Scanlan. J. Vet. Dent. December 2022; doi: 10.1177/08987564221141826. Quote: Medical records of dogs with dolico- or mesaticephalic conformation who were presented to a private veterinary referral dental practice with malocclusion of the deciduous or permanent dentition were retrospectively reviewed from a 3-year period (2015-2018). Records were evaluated to determine the type(s) of malocclusions and 198 dogs were evaluated with permanent malocclusions. Of the dogs with deciduous malocclusions, 45 (60%) had variations of a MAL1, 28 (38%) had a MAL2, 13 (17.6%) had a MAL3, and four (5.4%) had a MAL4, with 19 (26%) having more than one type of malocclusion. Poodles, Labrador Retrievers, and Cavalier King Charles Spaniels consisted of 37 (50%) of the dogs with deciduous malocclusions. Fifty-five (74%) dogs proceeded with interceptive orthodontics. Of the dogs with permanent malocclusions, 128 (65%) had a variant of a MAL1, 60 (30%) had a MAL2, 75 (38%) had a MAL3, and 11 (5.6%) had a MAL4, with a MAL1 occurring concurrently with 49 (82%) MAL2 cases. The most common type of MAL1 was linguoversion of one or both mandibular canine teeth in 92 (72%) dogs. The five most commonly affected breeds with permanent malocclusions were Poodles, Labrador Retrievers, Chihuahuas, Pit Bull Terriers, and Cavalier King Charles Spaniels. Overall, 39 (18%) dogs presented with malocclusions observed in this study were associated with the Poodle breed and 20 (9%) dogs were associated with the Labrador Retriever breed. This trend among Poodle mixes and Labrador Retrievers supports a familial pattern to malocclusions.
A Retrospective Study of Ectopic Eruption in 35 Dogs. Emilia Barbara Klim, Lisa Alexandra Mestrinho, Jerzy Pawel Gawor. J. Vet. Dentistry. December 2022; doi: 10.1177/08987564221141989. Quote: Ectopic eruption results from a disturbance in tooth development and eruption, leading to an erupted or non-erupted tooth being in an unexpected anatomical location. This retrospective case series describes the location, position, form, and clinical signs associated with ectopic eruption in dogs. Thirty-five dogs [including one cavalier King Charles spaniel] (46 teeth) were diagnosed with ectopic eruption at three clinical practices during 2017-2020. The cases were described in terms of the location, the development and eruption status, the clinical signs, the consequences, and the treatment performed. The collected data were statistically analyzed to establish possible ramifications. The results showed that the ectopic eruption in the evaluated cases involved permanent teeth, mainly located in the maxilla, and mostly unerupted. Those located in the mandible were significantly more impacted than those located in the maxilla. This study concluded that tooth crowding and malocclusion (39.1%), facial swelling (8.6%), and periodontal disease (8.6%) were associated with the presence of ectopic eruption, and consequently, treatment was required in the majority (65.2%) of cases.
Ascophyllum nodosum as a nutrient supporting oral health in dogs and cats: a review. J Gawor, M Jank. Polish J. Vet. Sci. September 2023; doi: 10.24425/pjvs.2023.145053. Quote: Home dental care is a key element of periodontal therapy in veterinary patients. Among many strategies of passive home dental care there is a supplementation of animal diet with seaweed Ascophyllum nodosum which have been shown to reduce both calculus and plaque accumulation after oral administration in both dogs and cats. Ascophyllum nodosum contains numerous biologically active ingredients, including micro-elements, vitamins, and several other compounds, however the exact mechanism of its beneficial action remains unclear. The very first metabolomic data suggest that it could change the composition of dog saliva. Several products containing Ascophyllum nodosum had been assessed clinically according to standards and requirements provided by the Veterinary Oral Health Council. The conducted clinical trials in dogs and cats revealed that Ascophyllum nodosum exerts the strongest preventive action as powder, followed by dental bites and dry pet food. The data concerning its curative action are limited to one study in cats in which no beneficial action has been observed. Based on available clinical data it is recommended to administer Ascophyllum nodosum to dogs and cats after oral cavity prophylactic procedure to reduce the recurrence of plaque and calculus formation.
The Presence of Bacteremia in 13 Dogs Undergoing Oral Surgery Without the Use of Antibiotic Therapy. Melissa Blazevich, Chanda Miles. J. Vet. Dentistry. November 2023; doi: 10.1177/08987564231207208. Quote: This study aimed to assess if transient bacteremia developed from dental scaling, root planing (SRP) and dental extraction(s), if the bacteria originated from oral flora, and if the amount of bacteremia produced would warrant the use of pre-, intra-, or post-operative antibiotic therapy in healthy canine patients. Blood cultures were obtained from 13 healthy dogs with chronic periodontal disease that necessitated the extraction of one tooth or multiple teeth. Patients included did not receive any antibiotic therapy for a minimum of 2 weeks prior to their scheduled procedure and did not receive antibiotic therapy intra- or post-operatively. Blood collection occurred at specific time increments to determine the presence of bacteremia and if clearance of the bacteremia occurred post-procedure. The study found transient bacteremia developed at different time increments throughout the dental procedure. At the time of the final sample collection, no bacterial growth was evident in any of the blood cultures. Results of the blood cultures indicated that only four of 13 dogs had evidence of bacterial growth at any one of the time increments; however, by the final collection, there was no bacterial growth suggesting the transient bacteremia had cleared without the use of systemic antimicrobial therapy. The study findings indicate that systemic antibiotic usage is not warranted for severe periodontal disease where an episode of transient bacteremia is produced from SRP and dental extractions in an otherwise healthy patient.
Preliminary evaluation of the impact of periodontal treatment on markers of glycaemic control in dogs with diabetes mellitus: A prospective, clinical case series. Ran Nivy, Yoav Bar-Am, Hanny Retzkin, Yaron Bruchim, Michal Mazaki-Tovi. Vet. Rec. January 2024; doi: 10.1002/vetr.3310. Quote: Background: Periodontal disease (PD) can adversely affect glycaemic control in humans. However, it is unknown if a similar association exists in dogs. Methods: Ten client-owned dogs with poorly regulated diabetes mellitus (DM) and PD were prospectively enrolled. A complete blood count, serum biochemistry, urinalysis and measurement of C-reactive protein, interleukin-6 (IL-6), tumour necrosis factor-a, haemoglobin A1c (HbA1c) and fructosamine concentrations were performed before periodontal treatment (PT) and monthly thereafter for 3 months. A periodontal disease severity score (PDSS) was determined during PT. The effects of time post-PT and PDSS on markers of inflammation and glycaemic control were determined by generalised estimating equation analysis. Results: HbA1c (mean; 95% confidence interval [CI]) decreased 3 months post-PT (32.1 mmol/mol; 21.1-43.1 mmol/mol vs. 44.3 mmol/mol; 36.4-52.0; p = 0.003). PDSS at enrolment was significantly (p = 0.031) positively associated with HbA1c concentration. Due to a significant (p < 0.001) interaction between PDSS and time post-PT in the analysis of fructosamine, dogs with low (1-3) PDSS and high (7-9) PDSS were analysed separately. Fructosamine (mean; 95% CI) significantly decreased 1 month post-PT (570 μmol/L; 457-684 μmol/L vs. 624 μmol/L; 499-748; p = 0.001) in the high PDSS group but not in the low PDSS group. Fructosamine concentration upon enrolment and PDSS were correlated (r = 0.73, p = 0.017). IL-6 concentration significantly decreased 3 months post-PT (9.9 pg/mL; 8.5-11.3 pg/mL vs. 11.2 pg/mL; 9.7-12.7; p = 0.002). Limitations: Limitations of the study included the small number of dogs, the lack of a control group and the inability to assess PDSS during follow-ups. Conclusions: These findings support a potential detrimental interaction between PD and DM. The apparent beneficial effect of PT on markers of glycaemic control was most conspicuous in dogs with more severe PD.
Intradental Displacement of a Deciduous Tooth Root in a Dog. Charlie Tewson, Simone Kirby. J. Vet. Dentistry. February 2024; doi: 10.1177/08987564241232856. Quote: This case study describes the diagnosis and treatment of a deciduous left maxillary canine tooth root that had been displaced into the pulp of the developing permanent left maxillary canine tooth in a 23-month-old female neutered Cavalier King Charles Spaniel. The patient was initially presented for bilateral persistent deciduous maxillary canine teeth extraction. Seventeen months later the permanent left maxillary canine tooth was found to be non-vital and tooth development had ceased prior to apical closure. Radiographs revealed a radio-opaque dentine-like structure and straight line centrally within the pulp of the permanent tooth. The displacement of the deciduous tooth into the developing permanent tooth was confirmed. This unusual potential complication should be considered when performing deciduous teeth extraction. ... Persistent deciduous teeth should be extracted as soon as the problem is identified, as abnormal orthodontic changes can occur within 2 weeks of permanent canine teeth erupting, and waiting until neutering before treating these teeth is inappropriate. 10 Pre- and postoperative radiographs should be performed.
Clinical evaluation of periodontal disease in dogs and cats. Tülay Koneçoğlu Sütlü. Balıkesir Univ. Health Sciences Institute. February 2024. Quote: Inflammation of the tissues that support and surround the tooth (gingiva, periodontal ligament, cementum, and alveolar bone) is classified as periodontal disease.In dogs and cats, periodontal disease results in loosening of teeth, halitosis, increased salivation, redness of the gums, loss of appetite, and tooth loss. Pets experiencing these symptoms may lose their appetite and suffer from a decline in overall health. In this thesis research, felines and canines that presented with periodontal disease were categorized based on their species, age, and gender attributes, and their periodontal disease stages were assessed and graded through clinical evaluations. Accurate diagnosis and treatment of periodontal disease require a comprehensive evaluation of clinical features such as gingival pocket depth measurements, radiographic imaging of the teeth, and other periodontal lesions. These assessments are critical in determining the extent and severity of the disease, enabling efficient and effective management of the condition. During our study, we examined the incidence of periodontal disease in cats and dogs. We considered various factors such as age, breed, gender, diet, and home care. After conducting research on 23 cats and 16 dogs [including 3 cavalier King Charles spaniels (18.75%)], we observed a trend among pets fed with dry food to develop periodontal disease. While each of the cases in the study had halitosis, it was observed that 90% of the complaints they brought to the clinic had the same symptoms. While periodontal disease is quite common in premolar teeth in cats, this similarity has not been observed in dogs; despite being carnivores, there are differences on a species basis. ... Nine out of 16 patients brought to the clinic (56.25%) were small breeds, and breeds that are prone to periodontal disease are Cavalier King Charles, Yorkshire Terrier, Pomeranian and Pekingese. ... The tendency to this disease in small breed dogs such as Pekingese, Yorkshire Terrier, Pomeranian, Cavalier was also seen in this study. ... As a result of the response received from the dog owners, 6 out of 16 dogs (37.5%) had difficulty eating [dry] food and dropped the food from their mouths. ... Periodontal disease is most commonly seen in animals that have moved away from their natural habitats, especially in cats and dogs that consume dry food and are fed with home food. ... In this study, all of the cats and dogs brought to our clinic are fed dry food. ... As a result of the survey conducted with patient owners, the tendency of cats and dogs fed dry food to periodontal disease was positively associated, as revealed in previous studies. ... Regular dental brushing has been found to support significant treatment in patients who are still in the early stages of the disease, even while differences in the antibiotics used in medical treatment do not yield substantial differences in outcomes. The study has revealed the significance of tooth brushing, particularly for pet owners with dogs and cats. Regular tooth brushing habit is necessary to protect against diseases, and it can be therapeutic in the early stages of the disease.
Persistent deciduous teeth: Association of prevalence with breed, breed size and body weight in pure-bred client-owned dogs in the United States. C. Wallis, A. Ivanova, L.J. Holcombe. Research Vet. Sci. March 2024; doi: 10.1016/j.rvsc.2024.105161. Quote: Dogs use their teeth for a multitude of tasks and, as such, it is vital for their health and wellbeing that their oral health is maintained. Persistent deciduous teeth (PDT), those that fail to fall out at the appropriate time, are associated with malocclusion (misaligned bite), soft tissue trauma and increased risk of periodontal disease. The objective of the current study was to perform a retrospective analysis of veterinary medical data to understand the effect of dog breed size, dog breed and body weight on prevalence of PDT. Medical records collected from almost 3 million dogs visiting a chain of veterinary hospitals across the United States over a 5-year period showed an overall prevalence of 7% for PDT, the data represented 60 breeds with extra-small breeds (<6.5 kg) showing significantly higher prevalence (15%) than all other breed sizes (P < 0.001). ... Cavalier King Charles spaniel also had higher odds of PDT compared to all other breeds within the size category with the exception of pug. ... The Cavalier King Charles spaniel, also a brachycephalic breed in the medium-small breed category, ranked second to the Pug for PDT prevalence at 5.5%. ... Statistical modelling of extra-small, small and medium-small breed sizes showed that those on Wellness Plans or that had not received a dental prophylaxis for at least two years had significantly increased odds of PDT being detected (Odds ratio 2.72-3.2 and 2.17-3.36 respectively, P < 0.0001). Dogs with a below ideal body condition score had a decreased odds of PDT (Odds ratio 0.57-0.89, P < 0.0001) whereas those above ideal had an increased odds (Odds ratio 1.11-1.60, P < 0.0001). The findings from this extensive dataset highlight the importance of regular veterinarian examinations to identify and remove PDT, helping to avoid increasing the risk of associated issues such as periodontal disease and malocclusion.
A Case Report of Periodontal Disease in a Dog. Silva R. Alves, Paolo Ruggero Errante. Int'l J. Zoology & Anim. Biology. January 2025; doi: 10.23880/izab-16000639. Quote: Periodontal disease is the most common condition affecting the oral cavity of dogs, characterized by gingivitis and periodontitis, caused by the presence of aerobic bacteria that accumulate on the surface of tooth in form of biofilm, subsequently favoring the colonization and growth of anaerobic bacteria with pathogenic potential. In gingivitis, inflammation of gums occurs, and in periodontitis, loss of epithelial adhesion, progressive bone loss and tooth mobility occur. Numerous factors are associated with periodontal disease, such as race, age, dental arch occlusion disorders, retention of deciduous teeth and dental crowding. The most common clinical signs of periodontal disease are halitosis and gum inflammation. The diagnosis is made through direct visual examination, which can identify the presence of dental calculus deposition and gingival inflammation, and the use of imaging tests such as radiography and computed tomography is essential. Surgical treatment consists of complete removal of dental calculus, removal of unstable teeth and polishing of teeth.In this study, a report of periodontal disease was carried out in a Cavalier King Charles Spaniel dog, which presented a large amount of supragingival dental calculus on all teeth. ... In October 2024, an 8-year-old male Cavalier King Charles Spaniel was seen, whose tutor main complaint was halitosis, the presence of dental calculus and oral bleeding after brushing of dog's teeth. The tutor reported that the animal had never undergone dental treatment and that he brushed the dog's teeth sporadically. During the clinical examination of the oral cavity, it was possible to observe accumulation of dental calculus and associated gingivitis. ... Tooth mobility was observed in the lower and upper incisor teeth, the first upper left premolar and the third lower left premolar, indicating the presence of advanced periodontal disease in some of these teeth. ... The diagnosis was made through clinical signs, physical examination and computed tomography with 3D imaging. Based on the findings of clinical evaluation and tomography, teeth with bone loss of supporting tissue were identified. The animal was anesthetized to remove the dental calculus and extract teeth that were mobile. ... All affected teeth were also polished to remove stains. ... The antibiotics clindamycin, metronidazole and spiramycin are normally used. Antibiotic therapy should begin three days before the surgical procedure and must be continued for next seven days after the procedure. In this case report, a combination of antibiotics metronidazole and spiramycin was used, three days before and seven days after surgery, obtaining a good clinical result. Antibiotic therapy brings several benefits, such as reducing local inflammatory response, reducing bleeding caused by scraping, reducing halitosis and reducing of oral microbial load associated with the formation of biofilm and dental calculus.
Modifiable early life risk factors for dental calculus in dogs: a retrospective cross-sectional study in Finland. Manal B. M. Hemida1, Sarah Holm, Mia Eklundh, Anna Hielm-Bjorkman. BMC Vet. Res. July 2025; doi: 10.1186/s12917-025-04885-8. Quote: Background: Dental calculus (DC) in dogs is a common oral health issue that can result in discomfort and may lead to systemic complications, if not managed effectively. While dental care practices are often overlooked by many owners, it remains crucial to identify and address possible DC risk and protective factors. The present retrospective cross-sectional study sought to examine the early life factors contributing to the emergence of owner-reported DC in dogs later in life, emphasizing the impact of modifiable variables. The study examined exposure data across five pivotal early life stages, starting prenatally and extending into adolescence. Multivariate logistic regression analyses using backward stepwise deletion were performed using data from 4771 dogs, including 2360 cases and 2411 controls, to examine the potential associations between DC in dogs and 29 distinct early life variables across five statistical models. The study incorporated a range of independent variables, including dietary, environmental, demographic, domestic, and immune-related factors. Additionally, the study aimed to compare between energy value and macronutrient composition of non-processed meat-based diets and ultra-processed carbohydrate-based diets available on the Finnish market. Results: Our research indicated that dogs fed a non-processed meat-based diet during the weaning period, puppyhood, and adolescence, which corresponds to the age range of 1 month to 1 or 1.5 years, were associated with a significantly lower risk of developing DC later in life. Conversely, dogs consumed an ultra-processed carbohydrate-based diet during the same periods was associated with a significantly higher risk (p = 0.01, p = 0.001, and p = 0.02 for weaning, puppyhood, and adolescence, respectively). Additionally, residing with other dogs was significantly associated with a decreased likelihood of DC development later in life (p = 0.015). Moreover, from the non-modifiable factors model, a maternal history of DC and small size of the dog were strongly associated with an increased risk of DC development later in life. Conclusions: ... In summary, the present study underscores the significance of early life exposures in modulating the risk of DC development in dogs later in life. We found that dogs fed a NPMD diet during weaning, late puppyhood and adolescence showed a significantly lower risk of developing DC later in life, whereas those consuming UPCD had a significantly higher risk. Moreover, living with other dogs was also significantly associated with a lower risk of DC development later in life. Additionally, the maternal history of DC was strongly associated with a high risk of DC development in offspring during adulthood, compared to dogs without a maternal history of DC, however it remains unclear whether shared genetic or environmental factors are primarily responsible. Furthermore, dogs belonging to small breeds and older dogs were significantly more susceptible to develop DC later in life, than dogs belonging to medium or large breeds and younger dogs. Although the current study suggests an association between early life exposures and later onset of DC in dogs, further longitudinal dietary interventions are required to verify our observations.
Anesthesia-free dentistry does not provide any demonstrable medical benefit for the control of periodontal disease in dogs. Brook A. Niemiec, Katherine B. Kangas, Erin P. Ribka. J. Amer. Vet. Med. Assn. October 2025; doi: doi.org/10.2460/javma.25.06.0405. Quote: Objective: To determine the effectiveness of anesthesia-free dentistry (AFD) versus anesthetic dentistry for treatment of periodontal disease in dogs. Methods: This prospective study was conducted between April 16, 2014, and October 21, 2014. Client-owned dogs were assigned an initial periodontal diagnostic test strip (PDTS) score (from 0 [white] to 5 [dark yellow]) during conscious oral examination using commercially available rapid test strips to assess salivary concentration of thiols (OraStripdx; PDX Biotech LLC). Eligible dogs included those with PDTS score > 3 and no previous dental cleaning (control group) and those with any PDTS score and a history of AFD in the previous 6 weeks. Because of this timeframe, the initial PDTS scores for the experimental group also served as a post-AFD PDTS score. All dogs in the control group and 14 of 23 dogs in the experimental group underwent anesthetized dental procedures. Periodontal disease was assessed under anesthesia, and PDTS scores were reassessed at recheck examination. Results were compared between groups. Results: 46 dogs were included, 23 in each group [including 2 cavalier King Charles spaniels in Group 1]. Mean PDTS score was significantly lower at recheck examination after anesthetic dentistry for both groups. Mean initial PDTS score did not differ significantly between groups; however, the mean PDTS score at recheck examination was significantly lower for dogs after an anesthetized dental procedure (0.087; range, 0 to 1) versus AFD (4.35; range, 3 to 5). Conclusions: No medical benefit was provided by AFD.


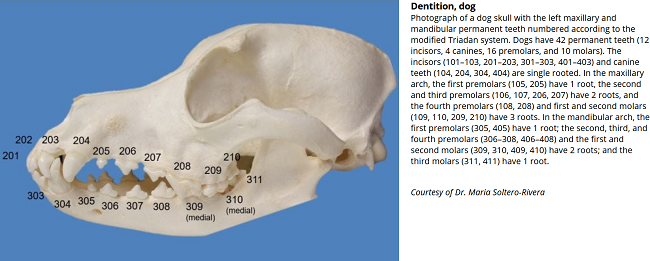
CONNECT WITH US