Chronic Pancreatitis and
the Cavalier King Charles Spaniel
-
 What It Is
What It Is - Symptoms
- Diagnosis
- Related Disorders
- Treatment
- What You Can Do
- Research News
- Related Links
- Veterinary Resources
The cavalier King Charles spaniel has a high prevalence of chronic pancreatitis and is believed to be predisposed to this disease, according to several recent reports. In a 2005 report by UK researchers, they found:
"There are strong breed-associations in CKCS and JRT, suggesting a possible genetic basis to the disease in these breeds."
This breed association has been confirmed in a 2007 UK report.*
* See also this 2007 UK report and this 2011 US report and this 2013 UK report.
Most cavaliers diagnosed with chronic pancreatitis are middle-aged or older. In a November 2014 presentation by Dr. Penny Watson, she stated that she has found the prevalence of chronic pancreatic disease in cavaliers to be as high as 80%.
What It Is
The pancreas is a gland which consists of about 98% exocrine acinar cells and 2% endocrine islets. The exocrine cells secrete enzymes* which aid the digestion of protein in the smaller intestine. The endocrine cells secrete insulin, which helps control carbohydrate metabolism, and glucagon, which offsets the action of the insulin.
* Enzymes secreted include lipase, alpha-amylase, phospholipase and the proteolytic enzymes elastase, chymotrypsin, and trypsin.
 A normally functioning pancreas is protected from premature activation of
these caustic digestive enzymes, which could result in digesting the
pancreas itself. Pancreatitis occurs when the enzymes are activated
while still in the pancreas, thereby causing death to its tissue by
auto-digestion.
A normally functioning pancreas is protected from premature activation of
these caustic digestive enzymes, which could result in digesting the
pancreas itself. Pancreatitis occurs when the enzymes are activated
while still in the pancreas, thereby causing death to its tissue by
auto-digestion.
Pancreatitis is a common inflammatory disorder of the dog's pancreas, which can be either "acute" or "chronic". Acute pancreatitis is an inflammation which does not cause permanent damage to the pancreas and therefore is potentially reversible. Chronic pancreatitis, for which the cavalier appears predisposed and is at an increased risk, is a continuous inflammation which can cause permanent damage to the pancreas’ exocrine and endocrine tissues and result in insufficient creation and secretion of its enzymes, particularly an exocrine pancreatic insufficiency (EPI).
The end stage of chronic pancreatitis may result in diabetes mellitus, due to extensive destruction of pancreatic tissues. In a January 2015 report, UK author Lucy J. Davison has observed that cases of diabetes mellitus often accompany exocrine pancreatic inflammation. She states:
"However, the question remains as to whether the diabetes mellitus causes the pancreatitis or whether, conversely, the pancreatitis leads to diabetes mellitus – as there is evidence to support both scenarios. The concurrence of diabetes mellitus and pancreatitis has clinical implications for case management as such cases may follow a more difficult clinical course, with their glycaemic control being 'brittle' as a result of variation in the degree of pancreatic inflammation. Problems may also arise if abdominal pain or vomiting lead to anorexia. In addition, diabetic cases with pancreatitis are at risk of developing exocrine pancreatic insufficiency in the following months to years, which can complicate their management further."
Contrary to earlier belief, no evidence has been found that high fat diets cause pancreatitis. However, because fat is harder to digest than other ingredients, researchers have found that high fat diets tend to increase the symptom of pain in dogs which already have chronic pancreatitis.
In this July 2013 article, a cavalier was diagnosed with acute pancreatitis, along with acute zinc toxicity following ingesting a metallic object which also resulted in hemolytic anemia.
RETURN TO TOP
Symptoms
The range of signs of chronic pancreatitis in cavaliers is from mild to severe. Classic signs include:
• abdominal pain
• vomiting
• diarrhea
• decrease/loss of appetite
• depression
• dehydration
• fever
• jaundice
• shortness of breath (dysspnea)
• weakness/lethargy
• shock
The pain can be severe and may cause the dog to take a “praying” position. The affected dog may also pass diarrhea or voluminous feces, with small amounts of fresh blood and/or mucous.
The clinical signs of pancreatitis may come and go, and they will vary with the severity of the disease. Low-grade cases may not show all of the classic symptoms and may be confused with inflammatory bowel disease or a chronic infection, such as a urinary tract infection. In severe cases, the dog may become dehydrated, may collapse, be in shock, and may even suffer renal shutdown and distressed breathing.
If a dog which has diabetes mellitus suddenly begins to lose weight unexpectedly, despite having a good appetite and being under diabetic control, the dog may have developed an exocrine pancreatic insufficiency (EPI) due to pancreatitis.
RETURN TO TOP
Diagnosis
Low grade chronic pancreatitis can be difficult to diagnose because their symptoms can be confused easily with other conditions. Recent studies have found a high rate of under-diagnosis of chronic pancreatitis in dogs. Initial diagnostic testing typically includes CBC blood panels, serum chemistry profile, urinalysis, and most recently, enzyme assays such as SNAP cPL.
-- enzyme assays
Enzyme assays -- catalytic, immuno, and enzymatic -- involve measuring levels of circulating pancreatic enzymes, including lipase, amylase, trypsin (cTLI), and canine pancreas specific lipase (cPLI). Measurement of elevated circulating enzymes, including amylase, lipase, cTLI, and cPLI currently are the best tests available for diagnoses. Nevertheless, no such assays have been found useful to assess for spontaneous pancreatitis.
 Researchers are constantly seeking to improve the accuracy of diagnosing
pancreatitis. IDEXX Laboratories claims that its SPEC cPL test,
a quantitative immunoassay, is the most
accurate, even more so than ultrasounds. See the
IDEXX website for details.
However, the Spec cPL results reportedly take at least 24 hours to return,
which can be an important limitation for some patients.
Researchers are constantly seeking to improve the accuracy of diagnosing
pancreatitis. IDEXX Laboratories claims that its SPEC cPL test,
a quantitative immunoassay, is the most
accurate, even more so than ultrasounds. See the
IDEXX website for details.
However, the Spec cPL results reportedly take at least 24 hours to return,
which can be an important limitation for some patients.
IDEXX Labs also offers a SNAP cPL test (right), a semiquantitative cPL immunoassay, for diagnosing pancreatitis. See the IDEXX website for details. In a July 2012 report of a comparison of various cPLI tests on 84 dogs, the researchers found that:
"SNAP and SPEC have higher sensitivity for diagnosing clinical AP [acute pancreatitis] than does measurement of serum amylase or lipase activity. A positive SPEC or SNAP has a good positive predictive value (PPV) in populations likely to have AP and a good negative predictive value (NPV) when there is low prevalence of disease."
The study was sponsored by IDEXX, the producer of SNAP and SPEC tests.
The SNAP cPL test is considered to be a rapid point-of-care semiquantitative cPL immunoassay which permits a more rapid return of results. The SNAP cPL test can be used to rapidly rule out pancreatitis, and it is recommended that a positive result be followed by laboratory assessment using a quantitative immunoassay, such as the Spec cPL.
The VetScan cPL Rapid Test has been developed by Abaxis Laboratories, with the aim of combining the benefits of a quantitative assay with the point-of-care benefits of the SNAP cPL. The VetScan cPL is a semiquantitative immunoassay for the detection of cPL that gives rapid point-of-care results. Unlike the SNAP cPL, the results of this point-of-care assay are numerical rather than binary, and is able to distinguish between patients without pancreatitis, those with equivocal results, and those with cPL results consistent with pancreatitis.
Non-immunologic colorimetric lipase assays are also available. The Precision PSL Test by Antech Diagnostics is a non-immunologic colorimetric lipase assay which utilizes the substrate 1,2-o-dilauryl-rac-glycero-3-glutaric acid (6'-methyl-resorufin) ester (DGGR), which has been validated for the diagnosis of acute pancreatitis in dogs. See this March 2005 article. In this May 2015 abstract, the researchers found that the DGGR-based assay is not specific for pancreatic lipase. However, in this April 2018 article, the researchers found that "DGGR lipase is a reliable alternative to Spec cPL for the diagnosis of pancreatitis."

In a November 2015 article, a group of Japanese researchers examined the use of a new diagnostic laboratory test, Fuji Dri-Chem lipase (FDP lip), compared to amylase, in diagnosing acute pancreatitis (AP). They found that among 64 dogs, activities of amylase and FDC lip were significantly higher in the AP group than in the nonpancreatic disease (NP) group. They report that the sensitivity of FDP lip activity for diagnosing AP was 100%. They did not compare the FDC lip with IDEXX's SNAP cPL test. They concluded that "the measurement of FDC lip activity appears useful for diagnosing AP."
In a July 2015 study, Spanish researchers report finding that some dogs treated with anticonvulsants (phenobarbital and potassium bromide) may show an increase in canine pancreas-specific lipase, but its increase may not be associated with severe acute pancreatitis.
Other diagnostic tests are being studied, including peptides in the blood and urine, and levels of inflammatory mediators and cytokines in the blood.
RETURN TO TOP
-- ultrasound
Ultrasounds can be very specific for pancreatitis, depending upon the extent of inflammation, when performed by skilled operators. Therefore, pancreatic ultrasounds should be performed by ultrasound specialists. Low grade chronic pancreatitis is the most difficult to detect using ultrasound. The rate of accuracy of detecting the disorder by ultrasound is about 60% overall and higher by skilled operators using high quality equipment.
Ultrasound scans can detect pancreatic swelling, changes in echogenicity of the pancreas, fluid accumulation around the pancreas, and a mass effect in the area of the pancreas.
In a March 2022 article, UK veterinary researchers studied 66 dogs diagnosed with acute pancreatitis (AP), including 3 cavaliers (4.55%). They sought to determine by ultrasound any gastrointestinal (GI) wall changes in the dogs, especially whether the presence of neutrophilia, left shift, or toxic neutrophils would serve as markers of increased severity of inflammation.They found that 31 of the dogs (47%) had ultrasonographic gastrointestinal wall changes, most commonly in the duodenum. Of the dogs with gastrointestinal wall changes, 23 (74.2%) had wall thickening, 19 (61.3%) had abnormal wall layering, and 11 (35.5%) had wall corrugation. Only increased heart rates was an independent predictor of gastrointestinal wall changes, but because of possible other factors, they considered heart rate unlikely to be useful in indicating whether GI wall changes are likely to be present. They concluded that ultrasonographic gastrointestinal wall changes were relatively common in this population of dogs with AP and that the results may aid clinicians in interpreting ultrasonographic gastrointestinal wall abnormalities in dogs with AP.
RETURN TO TOP
-- biopsy
The “gold standard” for diagnosing pancreatitis is a biopsy by making an incision through the abdominal wall. Alternatives to biopsies include a fine needle aspiration (cytologic evaluation), blood tests, enzyme assays, x-rays, and ultrasounds. Usually blood counts, pancreatic enzyme assays and x-rays are conducted in combination, as any one alone would be insufficient to accurately diagnose chronic pancreatitis.
RETURN TO TOP
Related Disorders
- exocrine pancreatic insufficiency (EPI)
- mitral valve disease
- diabetes mellitus
- gastrointestinal disorders
- pancreatitis, panniculitis, polyarthritis syndrome (PPP)
- the serotonin connection
-- Exocrine pancreatic insufficiency (EPI)
See our webpage on EPI.
-- Mitral valve disease
There is evidence of a link between advanced stages of mitral valve disease and pancreatitis. In a January 2015 study of 62 dogs -- 40 with various stages of MVD and 22 healthy ones (none were cavaliers) -- South Korean researchers found an increase in serum canine pancreatic lipase immunoreactivity (cPLI) concentrations with the worsening of heart failure signs in the affected dogs. They concluded that pancreatic injury is associated with congestive heart failure (CHF) caused by MVD. They acknowledged that there were limitations to the study, primarily due to the number of dogs and the extent of the assessment of pancreatitis in the dogs. Nevertheless, they stated:
"Despite these study limitations, our study results clearly suggest that the increased serum PLI concentration, to levels accepted as indicating pancreatitis, is a common comorbidity with congestive heart failure. Therefore, regular check-up for serum PLI level is warranted for early detection of pancreatitis from chronic heart diseases."
In a July 2019 article, South Korean researchers tested MVD-affected dogs in all ACVIM stages of MVD to evaluate any relationships between the progression of MVD and levels of lipase (and N-terminal pro B-type natriuretic peptide -- NT-proBNP). No cavaliers were included in the 84-dog study. They report finding that over a two-year period, NT-proBNP showed a strong positive correlation with increasing stage of heart disease; lipase showed a mild positive correlation with heart disease stage.
-- Diabetes mellitus
The end stage of chronic pancreatitis may result in diabetes mellitus, due to extensive destruction of pancreatic tissues. In a January 2015 report, UK author Lucy J. Davison has observed that cases of diabetes mellitus often accompany exocrine pancreatic inflammation. She states:
"However, the question remains as to whether the diabetes mellitus causes the pancreatitis or whether, conversely, the pancreatitis leads to diabetes mellitus – as there is evidence to support both scenarios. The concurrence of diabetes mellitus and pancreatitis has clinical implications for case management as such cases may follow a more difficult clinical course, with their glycaemic control being 'brittle' as a result of variation in the degree of pancreatic inflammation. Problems may also arise if abdominal pain or vomiting lead to anorexia. In addition, diabetic cases with pancreatitis are at risk of developing exocrine pancreatic insufficiency in the following months to years, which can complicate their management further."
-- Gastrointestinal disorders
See our separate webpage on gastrointestinal disorders, including hemorrhagic gastroenteritis (HGE). Pancreatitis has been determined to be a cause of HGE.
-- Pancreatitis, panniculitis, and polyarthritis syndrome (PPP)
Pancreatitis, panniculitis, and polyarthritis syndrome (PPP) is a very rare syndrome both in humans and dogs. Its primary signs are development of dead skin tissues and painful lesions, and swollen joints, typically around the hind legs. There may be only mild or no gastrointestional symptoms. Nonetheless, the patient also is diagnosed with chronic pancreatitis. Panniculitis is a condtion affecting the panniculus (the fat layer beneath the skin), resulting in painful bumps and inflammation. Polyarthritis means arthritic conditions affecting several joints at the same time.
In a September 2024 article, a 10 year old female cavalier had abscesses on her hind legs, fever, lethargy, lameness, and chronic pancreatitis. Sterile nodular panniculitis was diagnosed and was treated with steroids, but after 11 months, lesions spread on the skin and the lameness worsened. The dog was euthanized, and a post-mortem examination found a pancreatic adenocarcinoma and confirmed pancreatitis, panniculitis, polyarthritis (PPP), and osteomyelitis (bacterial infection of the bones and bone marrow).
-- The serotonin connection
Dr. Penny Watson of the University of Cambridge, who has been studying pancreatitis in cavaliers for many years, opined at a presentation in November 2014 the hypothesis that there may be a relationship between the serotonin carried by blood platelets through the vascular system to various organs, particularly the pancreas, the kidneys, the liver, the central nervous system, and the mitral valves of the heart, all causing scarring of and other damage to the tissues of these organs. She stated:
"We had a theory that these dogs have an increased propensity to produce scar tissue, and that in fact they are doing it in multiple organs. So, there is so link between some of these diseases. ... When we look at the central nervous system in dogs with syringomyelia histologically, we find more fibrosis around blood vessels than you would normally find in a normal dog. ... We don't know what's causing the scarring in the pancreas. There is something causing it, and it seems to be coming up the ducts because that's where a lot of this is happening. And actually my theory at the moment is that it has something to do with the duct bacteria. And that theory has developed after seeing not one or two, but actually four or five cavaliers with chronic pancreatitis who respond very well to antibiotic therapy, metronidazole therapy specifically. And that's the sort of antibiotic that we use for overgrowth of bacteria in the small intestine, not the sort of antibiotic we use for other infections. And so I either think they've got gut bacteria coming up the duct, and perhaps their normal gut bacteria and it just that cavaliers' over-responding. Or, maybe there's something about their duct flora that's driving it, but I think there is a link there, somehow or another between the cavalier's gut flora and what's happening in the pancreas.
"Now why might they [cavaliers] be forming too much scar tissue? ... A current theory revolves around their platelets. Platelets are blood clotting cells. ... In cavaliers, about 50% of cavaliers in the UK have these macro-platelets, these jumbo platelets. ... Something in these cavaliers is stimulating these stellate cells to transform and produce lots of fibrous tissue. ... We noticed in cavaliers ... that there was a pattern of increased fibrosis in multiple organs, the kidneys particularly. Mitral valve disease isn't scarring. Mitral valve disease is myxomatous change. ... But the cells that produce that are valvular interstitial cells, and they are identical to the stellate cells in the pancreas. The current theory ... is that these little dogs might have something in their platelets that they are releasing when they are going through blood vessels into different organs that's tending to cause fibrosis. And our theory ... is that this might be serotonin, which is also known as 5-hydroxytryptamine, because platelets contain a bucket load of serotonin. ...
"We already know that some cavaliers have elevated levels of serotonin, that's been shown. We also already know that serotonin is central to converting those valvular interstitial cells into myofibroblasts. ... I think what was most compelling for me was the human side of it. There is a particular horrible syndrome in people called carcinoid syndrome. People who've got serotonin secreting tumors that they've got. ... They get pancreatic, liver, and kidney fibrosis and mitral valve disease. ... So in a nutshell, the hypothesis was these big floppy platelets release serotonin easily as they pass through vessels, leading to fibrosis in perivascular areas."
RETURN TO TOP
Treatment
Unless a specific cause has been determined, most cases of pancreatitis are treated to relieve the symptoms, especially abdominal pain. If the cause is known (more likely in acute cases than chronic ones), the treatment includes removing that cause.
Treatment of acute onset pancreatitis with IV fluids usually is administered, because fluids are needed to maintain the function of the pancreas and hydration. Most affected dogs are dehydrated. However, over-hydration must be avoided. Othere organs, especially the kidneys, liver, and respiratory system, must be monitored to avoid complications caused by the pancreatitis. Nutritional food also is essential early in the treatment process. Appetite stimulants may be necessary. Initially, a low fat diet is recommended.
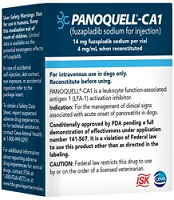 Fuzapladib sodium hydrate: In November 2022, the
USA's Food and Drug Administration (FDA) granted conditional approval of
fuzapladib sodium hydrate (Panoquell-CA1) for injection for the
management of clinical signs associated with acute onset of pancreatitis
in dogs. Panoquell-CA1 is an injectable drug intended for use while the
dog is hospitalized for treatment of the disease. Fuzapladib sodium, the
active ingredient in Panoquell, has been approved since 2018 in Japan to
improve clinical signs in the acute phase of pancreatitis in dogs. The
FDA reviewed data associated with fuzapladib’s use in Japan as part of
its assessment of the application for conditional approval. Fuzapladib
has not been studied in dogs with cardiac, hepatic, or renal disease;
dogs less than 6 months old; or dogs that are pregnant, lactating, or
intended for breeding. Among the
reported possible adverse effects are: gastrointestinal effects (eg,
anorexia, diarrhea, hypersalivation), hepatopathy, jaundice, respiratory
tract effects (eg, pneumonia, tachypnea, dyspnea), cardiac effects (eg,
arrhythmia, hypertension, cardiac arrest), hyperthermia, pruritus, and
cerebral edema. Conditional approval also means that, when used according to the label,
the drug is safe and has a reasonable expectation of effectiveness. The
drug sponsor must meet the requirements for substantial evidence of
effectiveness within five years for full approval.
Fuzapladib sodium hydrate: In November 2022, the
USA's Food and Drug Administration (FDA) granted conditional approval of
fuzapladib sodium hydrate (Panoquell-CA1) for injection for the
management of clinical signs associated with acute onset of pancreatitis
in dogs. Panoquell-CA1 is an injectable drug intended for use while the
dog is hospitalized for treatment of the disease. Fuzapladib sodium, the
active ingredient in Panoquell, has been approved since 2018 in Japan to
improve clinical signs in the acute phase of pancreatitis in dogs. The
FDA reviewed data associated with fuzapladib’s use in Japan as part of
its assessment of the application for conditional approval. Fuzapladib
has not been studied in dogs with cardiac, hepatic, or renal disease;
dogs less than 6 months old; or dogs that are pregnant, lactating, or
intended for breeding. Among the
reported possible adverse effects are: gastrointestinal effects (eg,
anorexia, diarrhea, hypersalivation), hepatopathy, jaundice, respiratory
tract effects (eg, pneumonia, tachypnea, dyspnea), cardiac effects (eg,
arrhythmia, hypertension, cardiac arrest), hyperthermia, pruritus, and
cerebral edema. Conditional approval also means that, when used according to the label,
the drug is safe and has a reasonable expectation of effectiveness. The
drug sponsor must meet the requirements for substantial evidence of
effectiveness within five years for full approval.
Mild cases of pancreatitis, with vomiting and dehydration, may require oral or intravenous fluids and pancreatic rest, meaning no solid food, followed by a change to a more appropriate diet. Hospitalization may be required to assure proper treatment and rest.
Antiemetics may be prescribed to reduce excessive vomiting, but they may have side effects which could increase pancreatic pain. A phenothiazine antiemetic such as chlorpromazine may avoid the additional pain, but it is not licensed for use by small animals. Cerenia (maropitant citrate) is an anti-nausea drug which is also a pain killer. Ondansetron, a 5-HT3 serotonergic antagonist, is another common medication for vomiting dogs.
Camostat mesilate, an oral protease inhibitor, has shown to be successful in rat studies to suppress pro-inflammatory cytokine production, markedly decrease microscopic signs of inflammation, and suppress fibrosis associated with chronic pancreatitis. It has been has been used clinically for the treatment of chronic pancreatitis in humans in Japan. In an April 2017 U.S. patent application, the inventors are seeking a patent to use camostat mesilate to treat dogs diagnosed with chronic panreatitis. In one study discussed in the application, two cavaliers were included among the dogs being treated.
Since pancreatitis is very painful, affected dogs may be given analgesia such as Paracetamol (acetaminophen)* or even a morphine agonist or partial agonist, particularly buprenorphine (Buprenex, Temgesic sublingual), or butophanol tartrate (Torbutrol, Stadol, Torbugesic-SA, Torbugesic). Non-steroidal anti-inflammatory drugs (NSAIDs) usually are not given because of an increased risk of gastroduodenal ulceration and a potential renal failure reaction. Vetergesic may be given by injection for severe pain. NSAIDs should not be administered without supervision by a veterinarian. The US Food & Drug Administration (FDA) warns about the dangers of using NSAIDs here on its website.
* Paracetamol (acetaminophen) can be toxic to dogs and must be given only under strict veterinary supervision.
While hospitalized, affected dogs may receive artificial nutrtion by enteral feeding (through a tube into the stomach or small intestine), which reportedly has been found to provide an early return to voluntary intake of food orally, to avoid the effects of delayed feedings upon the dogs' gastrointestinal systems.
A long-term low fat diet, along with supplementary enzymes, likely will be recommended. However, whether to feed the pancreatitis patient or not, and what to feed that patient, is so controversial that in this November 2016 article, the author reaches no specific conclusion. All dogs need fats in their diets. Less processed fats -- mainly uncooked fats rather than cooked fats -- appear to not cause or contribute to pancreatits.
Other veterinary nutritionists report that highly processed dry foods with high percentages of carbohydrates are either the cause of some cases or aggravate the dog's condition. They advise to give the pancreas a rest by initially fasting for one to two days. Then, follow up with small quantity meals -- 3 to 5 times a day -- instead of the usual two meals. Finally, they recommend avoiding dry foods entirely because they are highly processed and are very high in carbohyrates.
Severe cases, in which the tissue has begun to die (necrotize) and the liver has been affected, are unlikely to recover. However, in a 2009 review of the use of probiotics in veterinary practice, Dr. Susan G. Wynn reports that probiotics may benefit dogs with acute (but not chronic) necrotizing pancreatitis. She stated:
"Probiotic organisms appear to improve the intestinal barrier, which prevents bacterial translocation, and lactic acid–producing bacteria can suppress the inflammation that makes systemic inflammation response syndrome such a deadly condition in patients with acute pancreatitis. Investigators have conducted studies in dogs with experimentally induced severe pancreatitis. Affected dogs have been provided nutrients parenterally as well as elemental enteral nutrition or dietary supplementation with probiotics."
Dr. Penny Watson reported, in a November 2014 presentation, seeing some cavaliers with chronic pancreatitis "respond very well to antibiotic therapy, metronidazole* therapy specifically."
* Metronidazole (Flagyl) may cause adverse events in dogs hypersensitive to it. See Metronidazole Risks.
RETURN TO TOP
What You Can Do
Consider adding plant enzymes and probiotics to your dog's diet.
RETURN TO TOP
Research News
September 2024:
Cavalier is diagnosed with pancreatitis, panniculitis,
polyarthritis syndrome (PPP).
 In
a
September 2024 article, a team of Auburn University clinicians (Abby
Hagelskamp [right], Amelia G. White, Jeremy Gallman, Cierra
Starbird, Rachel L. A. L. T. Neto) report a case study of a 10 year old
female cavalier King Charles spaniel which had abscesses on her hind
legs, fever, lethargy, lameness, and chronic pancreatitis. Sterile
nodular panniculitis was diagnosed and was treated with steroids, but
after 11 months, lesions spread on the skin and the lameness worsened.
The dog was euthanized, and a post-mortem examination found a pancreatic
adenocarcinoma (a malignant glandular tumor) and confirmed
pancreatitis, panniculitis, polyarthritis (PPP), and osteomyelitis
(bacterial infection of the bones and bone marrow).
In
a
September 2024 article, a team of Auburn University clinicians (Abby
Hagelskamp [right], Amelia G. White, Jeremy Gallman, Cierra
Starbird, Rachel L. A. L. T. Neto) report a case study of a 10 year old
female cavalier King Charles spaniel which had abscesses on her hind
legs, fever, lethargy, lameness, and chronic pancreatitis. Sterile
nodular panniculitis was diagnosed and was treated with steroids, but
after 11 months, lesions spread on the skin and the lameness worsened.
The dog was euthanized, and a post-mortem examination found a pancreatic
adenocarcinoma (a malignant glandular tumor) and confirmed
pancreatitis, panniculitis, polyarthritis (PPP), and osteomyelitis
(bacterial infection of the bones and bone marrow).
March 2022:
Gastrointestinal wall changes were found in dogs diagnosed with
acute pancreatitis, in UK study.
 In
a
March 2022 article, UK veterinary researchers (Joshua J. Hardwick
[right], Elizabeth J. Reeve, Melanie J. Hezzell, Jenny A.
Reeve) studied 66 dogs diagnosed with acute pancreatitis (AP), including
3 cavaliers (4.55%). They sought to determine by ultrasound any
gastrointestinal (GI) wall changes in the dogs, especially whether the
presence of neutrophilia, left shift, or toxic neutrophils would serve
as markers of increased severity of inflammation.They found that 31 of
the dogs (47%) had ultrasonographic gastrointestinal wall changes, most
commonly in the duodenum. Of the dogs with gastrointestinal wall
changes, 23 (74.2%) had wall thickening, 19 (61.3%) had abnormal wall
layering, and 11 (35.5%) had wall corrugation. Only increased heart
rates was an independent predictor of gastrointestinal wall changes, but
because of possible other factors, they considered heart rate unlikely
to be useful in indicating whether GI wall changes are likely to be
present. They concluded that ultrasonographic gastrointestinal wall
changes were relatively common in this population of dogs with AP and
that the results may aid clinicians in interpreting ultrasonographic
gastrointestinal wall abnormalities in dogs with AP.
In
a
March 2022 article, UK veterinary researchers (Joshua J. Hardwick
[right], Elizabeth J. Reeve, Melanie J. Hezzell, Jenny A.
Reeve) studied 66 dogs diagnosed with acute pancreatitis (AP), including
3 cavaliers (4.55%). They sought to determine by ultrasound any
gastrointestinal (GI) wall changes in the dogs, especially whether the
presence of neutrophilia, left shift, or toxic neutrophils would serve
as markers of increased severity of inflammation.They found that 31 of
the dogs (47%) had ultrasonographic gastrointestinal wall changes, most
commonly in the duodenum. Of the dogs with gastrointestinal wall
changes, 23 (74.2%) had wall thickening, 19 (61.3%) had abnormal wall
layering, and 11 (35.5%) had wall corrugation. Only increased heart
rates was an independent predictor of gastrointestinal wall changes, but
because of possible other factors, they considered heart rate unlikely
to be useful in indicating whether GI wall changes are likely to be
present. They concluded that ultrasonographic gastrointestinal wall
changes were relatively common in this population of dogs with AP and
that the results may aid clinicians in interpreting ultrasonographic
gastrointestinal wall abnormalities in dogs with AP.
 October 2019:
Koreans find direct correlation between lipase levels in
progression of mitral valve disease in dogs. In a
July 2019 article, a team of Korean veterinary researchers (Jun-Seok
Park, Jae-Hong Park, Kyoung-Won Seo, Kun-Ho Song [right]) tested MVD-affected
dogs in all ACVIM stages of MVD to evaluate any relationships between
the progression of MVD and levels of lipase (and N-terminal pro B-type
natriuretic peptide -- NT-proBNP). No cavaliers were included in the
84-dog study. They report finding that over a two-year period, NT-proBNP
showed a strong positive correlation with increasing stage of heart
disease; lipase showed a mild positive correlation with heart disease
stage.
October 2019:
Koreans find direct correlation between lipase levels in
progression of mitral valve disease in dogs. In a
July 2019 article, a team of Korean veterinary researchers (Jun-Seok
Park, Jae-Hong Park, Kyoung-Won Seo, Kun-Ho Song [right]) tested MVD-affected
dogs in all ACVIM stages of MVD to evaluate any relationships between
the progression of MVD and levels of lipase (and N-terminal pro B-type
natriuretic peptide -- NT-proBNP). No cavaliers were included in the
84-dog study. They report finding that over a two-year period, NT-proBNP
showed a strong positive correlation with increasing stage of heart
disease; lipase showed a mild positive correlation with heart disease
stage.
February 2018:
Mississippi State Univ. researchers compare SNAP cPL, Spec cPL,
VetScan cPL, and Precision PSL enzyme assays for accuracy in diagnosing
pancreatitis in dogs.
 In a
February 2018 article, a team of five board-certified small animal
veterinary internists, led by Mississippi State University researchers
(Harry Cridge [right], A.G. MacLeod, G.E. Pachtinger, A.J. Mackin, A.M. Sullivant,
J.M. Thomason , T.M. Archer, K.V. Lunsford, K. Rosenthal, R.W. Wills),
compared the accuracy of four diagnostic assays -- SNAP canine
pancreatic lipase (cPL), specific cPL (Spec cPL), VetScan cPL Rapid
Test, and Precision PSL -- for pancreatitis in a group of 50 dogs. None
were cavalier King Charles spaniels. Their goal was to determine the
level of agreement among each of the four assays and a clinical
suspicion score, level of agreement among the assays, and sensitivity
and specificity of each assay in a clinically relevant group of dogs.
The clinical suspicion scoring was conducted by the five internists, on
a scale of 0 (the patient almost certainly did not have pancreatitis) to
2 (the patient almost certainly had pancreatitis) for each of the fifty
dogs and then averaged.
In a
February 2018 article, a team of five board-certified small animal
veterinary internists, led by Mississippi State University researchers
(Harry Cridge [right], A.G. MacLeod, G.E. Pachtinger, A.J. Mackin, A.M. Sullivant,
J.M. Thomason , T.M. Archer, K.V. Lunsford, K. Rosenthal, R.W. Wills),
compared the accuracy of four diagnostic assays -- SNAP canine
pancreatic lipase (cPL), specific cPL (Spec cPL), VetScan cPL Rapid
Test, and Precision PSL -- for pancreatitis in a group of 50 dogs. None
were cavalier King Charles spaniels. Their goal was to determine the
level of agreement among each of the four assays and a clinical
suspicion score, level of agreement among the assays, and sensitivity
and specificity of each assay in a clinically relevant group of dogs.
The clinical suspicion scoring was conducted by the five internists, on
a scale of 0 (the patient almost certainly did not have pancreatitis) to
2 (the patient almost certainly had pancreatitis) for each of the fifty
dogs and then averaged.
They found that:
• The level of agreement between individual diagnostic tests for pancreatitis and the clinical suspicion score was good.
• The level of agreement among the four diagnostic assays for pancreatitis was greater than the level of agreement between an individual diagnostic test and the clinical suspicion score.
• No single assay had high enough diagnostic specificity to conclusively diagnose pancreatitis based on a single test result, meaning that a combination of signalment, physical examination, blood tests, a pancreatic lipase test, and ideally, abdominal ultrasound examination, may be the most practical means of establishing a definitive diagnosis of clinical pancreatitis in dogs.
The study was funded by Abaxis Inc., the manufacturer of the VetScan cPL Rapid Test.
 April
2017:
Inventors seek US patent for chronic pancreatitis drug camostat
mesilate. In an
April 2017 U.S. patent application, the inventors (Long-Shiuh Chen,
Diana Wood, Aidan Nuttall) are seeking a
patent to use camostat mesilate to treat dogs diagnosed with chronic
panreatitis. In one study discussed in the application, two cavaliers
were included among the dogs being treated. Camostat mesilate is an oral
protease inhibitor which has been shown to be successful in rat studies
to suppress pro-inflammatory cytokine production, markedly decrease
microscopic signs of inflammation, and suppress fibrosis associated with
chronic pancreatitis. It has been has been used clinically for the
treatment of chronic pancreatitis in humans in Japan.
April
2017:
Inventors seek US patent for chronic pancreatitis drug camostat
mesilate. In an
April 2017 U.S. patent application, the inventors (Long-Shiuh Chen,
Diana Wood, Aidan Nuttall) are seeking a
patent to use camostat mesilate to treat dogs diagnosed with chronic
panreatitis. In one study discussed in the application, two cavaliers
were included among the dogs being treated. Camostat mesilate is an oral
protease inhibitor which has been shown to be successful in rat studies
to suppress pro-inflammatory cytokine production, markedly decrease
microscopic signs of inflammation, and suppress fibrosis associated with
chronic pancreatitis. It has been has been used clinically for the
treatment of chronic pancreatitis in humans in Japan.
November 2016:
To
feed or not to feed the pancreatitis patient?
Who
knows?
When a veterinary
 journal article title is in the form of a question,
you can be assured the author has no answer. In a
November 2016 article, a University of Florida veterinary
nutritionist (Justin Shmalberg, right) asks that question and ends up
raising
even more questions in his conclusion. For example, he states:
journal article title is in the form of a question,
you can be assured the author has no answer. In a
November 2016 article, a University of Florida veterinary
nutritionist (Justin Shmalberg, right) asks that question and ends up
raising
even more questions in his conclusion. For example, he states:
"Unfortunately, current knowledge is inadequate to provide a strong evidence-based recommendation on when and how to feed many patients."
"Dietary fat restriction appears to be a critical part of successful management of chronic disease in dogs, but its role in acute pancreatitis is less clear".
"The definition of a low fat diet for patients with pancreatitis is not well established".
January 2016:
Pancreatic lesions were found in 51.9% of post-mortem samples of
cavaliers in UK study.
 In an
April 2016 article, UK
researchers (Kent, Andrew C. C. [right]; Constantino-Casas, Fernando; Rusbridge,
Clare; Corcoran, Brendan; Carter, Margaret; Ledger, Tania; Watson, Penny
J.) searched for pancreatic, hepatic (liver) and renal (kidney) lesions
in post-mortem samples from 54 cavalier King Charles spaniels (CKCSs). The
rate of diagnosis of pancreatic disease prior to death was in 25% of the
CKCSs, but the post-mortem examination found evidence of chronic
pancreatitis in 51.9% of the dogs, and the dogs' ages correlated with
severity of disease. The researchers report that this evidence suggested
that chronic pancreatitis is a progressive condition. They concluded
that pancreatic lesions are common in the breed, and that clinicians should
be aware of this when presented with clinical cases.
In an
April 2016 article, UK
researchers (Kent, Andrew C. C. [right]; Constantino-Casas, Fernando; Rusbridge,
Clare; Corcoran, Brendan; Carter, Margaret; Ledger, Tania; Watson, Penny
J.) searched for pancreatic, hepatic (liver) and renal (kidney) lesions
in post-mortem samples from 54 cavalier King Charles spaniels (CKCSs). The
rate of diagnosis of pancreatic disease prior to death was in 25% of the
CKCSs, but the post-mortem examination found evidence of chronic
pancreatitis in 51.9% of the dogs, and the dogs' ages correlated with
severity of disease. The researchers report that this evidence suggested
that chronic pancreatitis is a progressive condition. They concluded
that pancreatic lesions are common in the breed, and that clinicians should
be aware of this when presented with clinical cases.
November 2015: Japanese clinicians find Fuji Dri-Chem lipase aided diagnosis of acute pancreatitis. In a November 2015 article, a group of Japanese researchers examined the use of a new diagnostic laboratory test, Fuji Dri-Chem lipase (FDP lip), compared to amylase, in diagnosing acute pancreatitis (AP). They found that among 64 dogs, activities of amylase and FDC lip were significantly higher in the AP group than in the nonpancreatic disease (NP) group. They report that the sensitivity of FDP lip activity for diagnosing AP was 100%. They did not compare the FDC lip with IDEXX's SNAP cPL test. They concluded that "the measurement of FDC lip activity appears useful for diagnosing AP."
July 2015: Spanish study shows anticonvulsants may cause increase in canine pancreas-specific lipase but not acute pancreatitis. In a July 2015 study, Spanish researchers (Mariana Teles, Antonio Meléndez-Lazo, Jaume Rodón, Josep Pastor) report finding that some dogs treated with anticonvulsants (phenobarbital and potassium bromide) may show an increase in canine pancreas-specific lipase, but its increase may not be associated with severe acute pancreatitis.
February 2015: Swedish study finds serotonin levels increase in spayed bitches. In a February 2015 report by veterinary doctoral student Elin Larsson, she studied 7 female dogs and 3 males, including on cavalier King Charles spaniel male, she found that "Among the bitches, the serotonin levels tended to increase after castration [sic]. The male dogs were few in number and no obvious changes in hormone levels were shown."
January 2015: Korean researchers find link between advanced MVD and pancreatitis. In a January 2015 study of 62 dogs -- 40 with various stages of MVD and 22 healthy ones (none were cavaliers) -- a team of South Korean researchers (D. Han, R. Choi, and C. Hyun) found an increase in serum canine pancreatic lipase immunoreactivity (cPLI) concentrations with the worsening of heart failure signs in the affected dogs. They concluded that pancreatic injury is associated with congestive heart failure (CHF) caused by MVD. They acknowledged that there were limitations to the study, primarily due to the number of dogs and the extent of the assessment of pancreatitis in the dogs. Nevertheless, they stated:
""Despite these study limitations, our study results clearly suggest that the increased serum PLI concentration, to levels accepted as indicating pancreatitis, is a common comorbidity with congestive heart failure. Therefore, regular check-up for serum PLI level is warranted for early detection of pancreatitis from chronic heart diseases."
January 2015: "Pancreatitis
in Cavaliers: What is it and what can I do about it?" A DVD
(right)
 of
a seminar presented by Dr. Penny Watson of the University of Cambridge,
UK in November 2014, is available for purchase from Cavalier
Matters.
of
a seminar presented by Dr. Penny Watson of the University of Cambridge,
UK in November 2014, is available for purchase from Cavalier
Matters.
In her presentation, Dr. Watson reported finding a very high prevalence of chronic pancreatitis in cavaliers. Specifically, she said:
"What we've found, just looking at the histology, is that there is a very high prevalence, and that by the time we get to dogs of 11, 12, 13, I would be surprised to see a normal pancreas. And I would say the prevalence of chronic pancreatitis in cavaliers mimics mitral valve disease. ... I would say about 80%. ... Like mitral valve disease, it is a disease of aging. It is not so common in younger dogs."
She also discussed a current hypothesis which links mitral valve disease and pancreatitis and kidney disease in cavaliers through the secretion of serotonin by the cavaliers' blood platelets. She stated:
"We noticed in cavaliers ... that there was a pattern of increased fibrosis in multiple organs, the kidneys particularly. Mitral valve disease isn't scarring. Mitral valve disease is myxomatous change. ... But the cells that produce that are valvular interstitial cells, and they are identical to the stellate cells in the pancreas. The current theory ... is that these little dogs might have something in their platelets that they are releasing when they are going through blood vessels into different organs that's tending to cause fibrosis. And our theory ... is that this might be serotonin, which is also known as 5-hydroxytryptamine, because platelets contain a bucket load of serotonin. ... We already know that some cavaliers have elevated levels of serotonin, that's been shown. We also already know that serotonin is central to converting those valvular interstitial cells into myofibroblasts. ... I think what was most compelling for me was the human side of it. There is a particular horrible syndrome in people called carcinoid syndrome. People who've got serotonin secreting tumors that they've got. ... They get pancreatic, liver, and kidney fibrosis and mitral valve disease. ... So in a nutshell, the hypothesis was these big floppy platelets release serotonin easily as they pass through vessels, leading to fibrosis in perivascular areas."
January 2015: Which disorder causes the other? Diabetes mellitus or exocrine pancreatic inflammation? In a January 2015 report, UK author Lucy J. Davison has observed that cases of diabetes mellitus often accompany exocrine pancreatic inflammation. She states:
"However, the question remains as to whether the diabetes mellitus causes the pancreatitis or whether, conversely, the pancreatitis leads to diabetes mellitus – as there is evidence to support both scenarios. The concurrence of diabetes mellitus and pancreatitis has clinical implications for case management as such cases may follow a more difficult clinical course, with their glycaemic control being 'brittle' as a result of variation in the degree of pancreatic inflammation. Problems may also arise if abdominal pain or vomiting lead to anorexia. In addition, diabetic cases with pancreatitis are at risk of developing exocrine pancreatic insufficiency in the following months to years, which can complicate their management further."
January
2014:
Dr. Penny Watson looks for ties between fibrosis in MVD, SM, and chronic
 pancreatitis in CKCSs.
Dr. Penny Watson (right) of UK's Cambridge University's veterinary school is
spearheading a new study into whether several of the CKCS breed's hereditary
health problems are the result of the same genetic defect. Specifically, she
intends to explore the possibility that disparate cavalier diseases,
including mitral valve disease (MVD), syringomyelia (SM), and chronic
pancreatitis are connected at the cellular level by unusual patterns of
fibrotic changes. "Pronounced perivescular fibrosis", a feature in dogs with
chronic pancreatitis, also has been tied to a condition of the central
nervous system in cavaliers with SM. Dr. Watson has suggested that
deterioration of cavaliers' mitral valves also may be a result of a process
connected to the causes of fibrosis.
pancreatitis in CKCSs.
Dr. Penny Watson (right) of UK's Cambridge University's veterinary school is
spearheading a new study into whether several of the CKCS breed's hereditary
health problems are the result of the same genetic defect. Specifically, she
intends to explore the possibility that disparate cavalier diseases,
including mitral valve disease (MVD), syringomyelia (SM), and chronic
pancreatitis are connected at the cellular level by unusual patterns of
fibrotic changes. "Pronounced perivescular fibrosis", a feature in dogs with
chronic pancreatitis, also has been tied to a condition of the central
nervous system in cavaliers with SM. Dr. Watson has suggested that
deterioration of cavaliers' mitral valves also may be a result of a process
connected to the causes of fibrosis.
The CKCS breed's documented overabundance of serotonin, a neurotransmitter protein, has been identified as a plausible mechanism which may trigger the development of fibrotic changes in the heart's valves. Her study entails establishing primary stellate cell (SC) cultures from CKCS and define 5HT receptor subtype expression. Stellate cell (SC) activation is a key event in the development of hepatic and pancreatic fibrosis. Serotonin has been shown to activate SCs via 5HT receptors. The study is measuring the response of these cells to serotonin and other stimulators of fibrosis. She then intends to attempt to block SC activation in vitro using 5HTreceptor antagonists. Increased understanding of the factors driving fibrosis will be of benefit to the CKCS and may allow a drug trial in the breed.
March 2013: UK researcher seeks breakthroughs in understanding chronic pancreatitis in CKCSs. Dr. Penny Watson of the University of Cambridge is working closely with UK breeders of cavaliers to better understand the cause of chronic pancreatitis (CP) in the breed.* Over the past decade, she has published four research papers about CP, noting in the latter three its high prevalence in the CKCS. She also has found that the pathology of CP in the cavalier has a distinctive appearance. She said recently that "I hope we will soon be able to make some breakthroughs in understanding this disease better."
* See her 2004 report, her 2005 report, her 2007 report, and her 2012 report.
July
2012: Surprise! I DEXX finds that its SNAP and
SPEC tests are the best for diagnosing acute pancreatitis. In a
July 2012 report of a comparison
of various cPLI tests on 84 dogs, the researchers found that:
DEXX finds that its SNAP and
SPEC tests are the best for diagnosing acute pancreatitis. In a
July 2012 report of a comparison
of various cPLI tests on 84 dogs, the researchers found that:
"SNAP and SPEC have higher sensitivity for diagnosing clinical AP [acute pancreatitis] than does measurement of serum amylase or lipase activity. A positive SPEC or SNAP has a good positive predictive value (PPV) in populations likely to have AP and a good negative predictive value (NPV) when there is low prevalence of disease."
Of course, the study was sponsored by IDEXX, the producer of SNAP and SPEC tests. However, that fact is not intended to take anything away from the value of these two tests.
May 2011: Cavaliers and Jack Russells may be predisposed. US researchers report in a May 2011 study that cavalier King Charles spaniels are one of only two breeds which may be predisposed to chronic pancreatitis which can result in destruction of acinar cells. The other breed is the Jack Russell terrier (Parson Russell terrier in AKC).
March
2009: Probiotics may benefit dogs with acute necrotizing
pancreatitis. In a March 2009
 review
of probiotics in veterinary practice, Dr. Susan G. Wynn
(right) reports that probiotics may benefit dogs with acute necrotizing
pancreatitis. She writes:
review
of probiotics in veterinary practice, Dr. Susan G. Wynn
(right) reports that probiotics may benefit dogs with acute necrotizing
pancreatitis. She writes:
"Probiotic organisms appear to improve the intestinal barrier, which prevents bacterial translocation, and lactic acid–producing bacteria can suppress the inflammation that makes systemic inflammation response syndrome such a deadly condition in patients with acute pancreatitis. Investigators have conducted studies in dogs with experimentally induced severe pancreatitis. Affected dogs have been provided nutrients parenterally as well as elemental enteral nutrition or dietary supplementation with probiotics."
RETURN TO TOP
Related Links
RETURN TO TOP
Veterinary Resources
Control of Canine Genetic Diseases. Padgett, G.A., Howell Book House 1998, pp. 198-199, 232.
Pancreatitis in the dog: dealing with a spectrum of disease. Penny Watson. In Practice, Feb 2004; 26:64-77. Quote: "PANCREATITIS - whether it be acute or chronic - is a relatively common, but often misdiagnosed, problem in dogs. It is associated with a systemic inflammatory response which, in severe cases, can result in the development of multiorgan failure, diffuse intravascular coagulation and death. Classical acute pancreatitis is often straightforward to diagnose, but this only represents one end of a wide spectrum of disease. Milder and/or more chronic forms of the condition are not so easily recognised, but can cause significant pain and reduce the quality of life of an animal. There is no single diagnostic test with 100 per cent sensitivity and specificity for the disease, apart from biopsy which is relatively invasive and, hence, not often indicated. Treatment recommendations depend on the severity of the disease and range from conservative management at home to referral for intensive care. The causes of pancreatitis in dogs are usually unknown. Therefore, therapy tends to be symptomatic and non-specific. The potential long-term sequelae of chronic pancreatitis in dogs are largely uninvestigated, but can include the development of diabetes mellitus and/or exocrine pancreatic insufficiency. This article discusses the potential causes, diagnosis and treatment of acute and chronic pancreatitis in dogs."
Validation and diagnostic efficacy of a lipase assay using the substrate 1,2-o-dilauryl-rac-glycero glutaric acid-(6′methyl resorufin)-ester for the diagnosis of acute pancreatitis in dogs. Roberta Graca, Joanne Messick, Sheila McCullough, Anne Barger, Walter Hoffmann. Vet. Clin. Pathol. March 2005;34(1):39-43. Quote: Background: Increased serum lipase activity has been used historically to support the diagnosis of acute pancreatitis, a common disease in dogs. Most of the lipase assays that are currently in use lack optimum sensitivity and specificit-(6′-methylresorufin) ester (DGGR) assay for determination of lipase activity in canine serum and 2) compare results, reference intervals, sensitivity, and specificity of the DGGR assay with a standard 1,2-diglyceride (1,2 DiG) assay for diagnosing acute pancreatitis in dogs. Methods: Precision, linearity, and interference studies were performed for method validation on a Hitachi 911 analyzer. Lipase results from the DGGR and 1,2 DiG assays were compared by linear regression analysis. Sensitivity, specificity, and diagnostic efficacy were determined for both assays on a population of 30 dogs, 15 of which had acute pancreatitis based on history, clinical signs, and ultrasound findings. Results: Within-run and within-day coefficients of variation (CVs) were low (<3%), with higher day-to-day CVs (≤14 %). The assay was linear between 8 and 2792 U/L. No significant interference by hemolysis and lipemia was found. Poor correlation was found between the assays (rs= 0.84). The lipase reference interval was 8–120 U/L for the DGGR assay and 30–699 U/L for the 1,2 DiG assay. Sensitivity and specificity for the diagnosis of pancreatitis were 93% and 53%, respectively, for the DGGR assay and 60% and 73% for the 1,2 DiG assay. Receiver operating characteristic curve analysis showed similar areas under the curve. Conclusions: On the basis of this study, the DGGR method is considered adequate for assaying serum lipase activity in dogs. The high sensitivity of the DGGR assay suggests it may be a useful screening test for canine pancreatitis.
Prevalence of Chronic Pancreatitis at Post Mortem Examination in an Unselected Population of First Opinion Dogs. PJ Watson, A Roulois, P Johnston, H Thompson, ME Herrtage. ECVIM 2005 Symposium Absract # 69. J.Vet.Intern. Med.;19(6).Quote: "The prevalence of chronic pancreatitis (CP) dogs is unknown. Previous studies have focused on acute pancreatitis and/or have used a highly biased and selected population of second opinion and critical care cases. This study aimed to assess the prevalence of chronic pancreatitis in an unselected population of first opinion dogs. Sections were obtained from 100 consecutive canine post mortems presented to Glasgow Veterinary School from surrounding first opinion practices. Most dogs were assessed as middle-aged to old. In each case, 3 sections of pancreas were taken: one from each limb and one from the body. Sections were preserved in formalin and stained with H&E and Sirius red. They were examined histologically, blind to signalment. Clinical details were not available. The dogs were grouped according to histological findings: (a) sections too autolysed to interpret; (b) no abnormalities visible; (c) non specific/non significant changes; (d) chronic or acute-on-chronic pancreatitis; (e) acute pancreatitis with no chronic changes and (f) other disease. Prevalence of each group was calculated and relative risk of CP and autolysis were calculated for different breeds. Prevalence of autolysis was 27%, a shortcoming of this type of study. Autolysis was common in large breed dogs due to slow cooling of core temperature (e.g German shepherd dogs relative risk of autolysis 3.8) so relative risk of CP could not be calculated in large breeds. The pancreas had no histological abnormalities in only 13% of dogs. Non specific changes were observed in 24% of dogs. Acute pancreatitis had a low prevalence of 2%. The prevalence of CP was 29% and breeds with a high relative risk included Cavalier King Charles spaniels (CKCS): relative risk 4.1 and Jack Russell terriers: relative risk 2.4. 6/6 CKCS had CP, with 1/6 having end stage disease and 1/6 having concurrent pancreatic neoplasia. The lesions observed are likely to correlate with clinical disease: one out of four published cases of end stage CP with exocrine pancreatic insufficiency (EPI) was a CKCS and a further 2/7 biopsy-confirmed cases of chronic pancreatitis seen at the Queen’s Veterinary School Hospital since 2002 were CKCS, both of which had EPI and one of which had diabetes mellitus. We conclude that CP is common in the first opinion dog population and that, like in the liver, end stage disease can be considered as a distinct clinically significant entity. There are strong breed-associations in CKCS and JRT, suggesting a possible genetic basis to the disease in these breeds."
Diagnosing and Treating Pancreatitis: A roundtable discussion. David A. Williams, Jörg M. Steiner, H. Mark Saunders, David Twedt, Benita von Dehn. IDEXX Learning Center. 2006.
Prevalence and breed distribution of chronic pancreatitis at post-mortem examination in first-opinion dogs. P. J. Watson, A. J. A. Roulois, T. Scase, P. E. J. Johnston, H. Thompson, and M. E. Herrtage. J Small Animal Prac (2007) 48:609–618. Quote: Quote: "Objectives: To assess the prevalence of canine chronic pancreatitis in first-opinion practice and identify breed associations or other risk factors. Methods: Three sections of pancreas were taken from 200 unselected canine post-mortem examinations from first-opinion practices. Sections were graded for inflammation, fibrosis and other lesions. Prevalence and relative risks of chronic pancreatitis and other pancreatic diseases were calculated. Results: The prevalence of chronic pancreatitis was 34 per cent omitting the autolysed cases. Cavalier King Charles spaniels, collies and boxers had increased relative risks of chronic pancreatitis; cocker spaniels had an increased relative risks of acute and chronic pancreatitis combined. Fifty-seven per cent of cases of chronic pancreatitis were classified histologically as moderate or marked. Forty-one per cent of cases involved all three sections. Dogs with chronic pancreatitis were more commonly female and overweight, but neither factor increased the relative risk of chronic pancreatitis. There were breed differences in histological appearances and 24·5 per cent of cases were too autolysed to interpret with an increased relative risk of autolysis in a number of large breeds. Clinical Significance: Chronic pancreatitis is a common, under-estimated disease in the first-opinion dog population with distinctive breed risks and histological appearances."
Prognostic Factors in Canine Exocrine Pancreatic Insufficiency: Prolonged Survival is Likely if Clinical Remission is Achieved. Daniel J. Batchelor, Peter-John M. Noble, Rebecca H. Taylor, Peter J. Cripps, and Alexander J. German. J Vet Intern Med 2007;21:54–60. Quote: "Background: Response to therapy in canine exocrine pancreatic insufficiency (EPI) varies considerably, making it difficult to determine prognosis for individual patients. Hypothesis: Response to initial treatment (RIT) and survival are affected by signalment, clinical variables, and herapeutic regimen employed. Animals: Client-owned dogs diagnosed with EPI between 1990 and 2002 were included in this study. Methods: The study comprised a retrospective, questionnaire-based review. Results: One hundred seventy-eight completed questionnaires were returned [16 cavalier King Charles spaniels]]. RIT was good in 60% of treated dogs, partial in 17%, and poor in 23%. On univariate analysis, dogs that received antibiotics (P 5 .037) or had high serum folate concentration (P 5 .037) had a poorer RIT. On multivariate analysis, there were no strong predictors of good RIT. Nineteen percent of treated dogs were euthanized within 1 year, but overall median survival time for treated dogs was 1919 days. No clear benefit of changing to a fat-restricted diet could be demonstrated, but marked hypo-cobalaminemia (,100 ng/L) was associated with shorter survival (P 5 .012). Use of uncoated pancreatic enzyme supplements, antibacterials, or H2 antagonists was not associated with longer survival. Breed, sex, age at diagnosis (#4 years or .4 years), and clinical signs at diagnosis also made no difference. Conclusions and Clinical Importance: Long-term prognosis in canine EPI is favorable for dogs that survive the initial treatment period. Although there are few predictors of good RIT or long-term survival, severe cobalamin deficiency is associated with shorter survival. Therefore, parenteral cobalamin supplementation should be considered when hypocobalaminemia is documented."
Breed Associations for Canine Exocrine Pancreatic Insufficiency. Daniel J. Batchelor, Peter-John M. Noble, Peter J. Cripps, Rebecca H. Taylor, Lynn McLean, Marion A. Leibl, Alexander J. German. J. Vet. Intern. Med. March 2007;21(2):207–214. Quote: Background: Knowledge of breed associations is valuable to clinicians and researchers investigating diseases with a genetic basis. Hypothesis: Among symptomatic dogs tested for exocrine pancreatic insufficiency (EPI) by canine trypsin-like immunoreactivity (cTLI) assay, EPI is common in certain breeds and rare in others. Some breeds may be overrepresented or underrepresented in the population of dogs with EPI. Pathogenesis of EPI may be different among breeds. Animals: Client-owned dogs with clinical signs, tested for EPI by radioimmunoassay of serum cTLI, were used. Methods: In this retrospective study, results of 13,069 cTLI assays were reviewed. Results: An association with EPI was found in Chows, Cavalier King Charles Spaniels (CKCS), Rough-Coated Collies (RCC), and German Shepherd Dogs (GSD) (all P , .001). Chows (median, 16 months) were younger at diagnosis than CKCS (median, 72 months, P , .001), but not significantly different from GSD (median, 36 months, P 5 .10) or RCC (median, 36 months, P 5 .16). GSD (P , .001) and RCC (P 5 .015) were younger at diagnosis than CKCS. Boxers (P , .001), Golden Retrievers (P , .001), Labrador Retrievers (P , .001), Rottweilers (P 5 .022), and Weimaraners (P 5 .002) were underrepresented in the population with EPI. Conclusions and Clinical Implications: An association with EPI in Chows has not previously been reported. In breeds with early-onset EPI, immune-mediated mechanisms are possible or the disease may be congenital. When EPI manifests later, as in CKCS, pathogenesis is likely different (eg, secondary to chronic pancreatitis). Underrepresentation of certain breeds among dogs with EPI has not previously been recognized and may imply the existence of breed-specific mechanisms that protect pancreatic tissue from injury. ... There are strong breed associations with CP in the Cavalier King Charles Spaniel (CKCS) and Jack Russell Terrier. ... Breeds with increased prevalence: ... Cavalier King Charles Spaniel:: Number Affected [with EPI]: 64; Number Tested: 243.
Platelet function in dogs: breed differences and effect of acetylsalicylic acid administration. Line A. Nielsen, Nora E. Zois, Henrik D. Pedersen, Lisbeth H. Olsen, Inge Tarnow. Veterinary Clinical Pathology. September 2007;36(3):267-273. Quote: "Background: Clinical studies investigating platelet function in dogs have had conflicting results that may be caused by normal physiologic variation in platelet response to agonists. Objectives: The objective of this study was to investigate platelet function in clinically healthy dogs of 4 different breeds by whole-blood aggregometry and with a point-of-care platelet function analyzer (PFA-100), and to evaluate the effect of acetylsalicylic acid (ASA) administration on the results from both methods. Methods: Forty-five clinically healthy dogs (12 Cavalier King Charles Spaniels [CKCS], 12 Cairn Terriers, 10 Boxers, and 11 Labrador Retrievers) were included in the study. Platelet function was assessed by whole-blood aggregation with ADP (1, 5, 10, and 20 μM) as agonist and by PFA-100 using collagen and epinephrine (Col + Epi) and Col + ADP as agonists. Plasma thromboxane B2 concentration was determined by an enzyme immunoassay. To investigate the effect of ASA, 10 dogs were dosed daily (75 or 250 mg ASA orally) for 4 consecutive days. Results: A higher platelet aggregation response was found in CKCS compared to the other breeds. Longer PFA-100 closure time (Col + Epi) was found in Cairn Terriers compared to Boxers. Plasma thromboxane B2 concentration was not statistically different between groups. Administration of ASA prolonged the PFA-100 closure times, using Col + Epi (but not Col + ADP) as agonists. Furthermore, ASA resulted in a decrease in whole-blood platelet aggregation. Conclusions: Platelet function is influenced by breed, depending upon the methodology applied. However, the importance of these breed differences remains to be investigated. The PFA-100 method with Col + Epi as agonists, and ADP-induced platelet aggregation appear to be sensitive to ASA in dogs."
Canine Pancreatitis--From Clinical Suspicion to Diagnosis. Thomas Spillmann. 2008 WSAVA Congress. Quote: "Breeds with reported increased risk for chronic pancreatitis are cavalier King Charles and cocker spaniels, collies, and boxers."
Pancreatitis associated with clomipramine administration in a dog. P. H. Kook, A. Kranjc, M. Dennler, T. M. Glaus. J.Sm.Ani.Prac. 2009;50(1):95-98. Quote: "A three-year-old, male, entire, Yorkshire terrier was presented with peracute onset of abdominal pain and vomitus. Clinicopathological abnormalities included severely increased serum lipase activity, immeasurably high serum trypsin-like immunoreactivity and mild hypocalcaemia. Canine pancreatic lipase immunoreactivity (cPLI) was intended to be measured, however, the sample got lost. Ultrasonography revealed a hypoechoic pancreas with small amounts of peripancreatic fluid and hyperechogenic mesentery. Acute pancreatitis (AP) was diagnosed and the dog recovered with appropriate therapy within 48 hours. Clomipramine, a selective serotonin reuptake inhibitor (SSRI) for alleviating signs of separation anxiety had been given for seven weeks. Two similar, albeit less severe, episodes associated with previous courses of clomipramine had occurred eight months earlier that responded to discontinuing clomipramine and supportive care. As SSRIs are associated with AP in human beings and no other trigger could be identified, we conclude that clomipramine should be considered as a potential cause when investigating causes for AP in susceptible breeds or other dogs presenting with compatible clinical signs."
Probiotics in veterinary practice. Susan G. Wynn. JAVMA March 2009;234(5):606-613. Quote: "Pancreatitis: Translocation of gastrointestinal bacteria during pancreatitis can lead to septicemia and substantially worsen a patient’s prognosis. Results of studies conducted in humans and other animals by use of Lactobacillus plantarum 299, Saccharomyces boulardii, and combinations of probiotics and prebiotics suggest that probiotic administration may be of benefit in patients with acute necrotizing pancreatitis. Probiotic organisms appear to improve the intestinal barrier, which prevents bacterial translocation, and lactic acid–producing bacteria can suppress the inflammation that makes systemic inflammation response syndrome such a deadly condition in patients with acute pancreatitis. Investigators have conducted studies in dogs with experimentally induced severe pancreatitis. Affected dogs have been provided nutrients parenterally as well as elemental enteral nutrition or dietary supplementation with probiotics. In 1 study, increases in serum activity of amylase, alanine aminotransferase, and aspartate aminotransferase and plasma concentrations of endotoxin, as well as pancreatic and ileal histopathologic changes, were significantly (P < 0.05) suppressed with probiotic administration. The degree of bacterial translocation was significantly (P < 0.05) decreased with probiotic administration, which suggested that this probiotic combination (described as 40 mg of Lactobacillus spp and 40 mg of Bifidobacterium spp) enhanced gastrointestinal barrier function. Investigators in another study obtained similar results."
Breed Predispositions to Disease in Dogs & Cats (2d Ed.). Alex Gough, Alison Thomas. 2010; Wiley-Blackwell Publ. 52.
Prevalence of hepatic lesions at post-mortem examination in dogs and association with pancreatitis. P. J. Watson, A. J. A. Roulois, T.J. Scase1, R. Irvine, M. E. Herrtage. J. Sm. An. Prac. Nov 2010;51(11):566–572. Quote: "To assess the prevalence of canine chronic hepatitis (CH) and other liver diseases in first opinion practice and identify associations with concurrent chronic pancreatitis (CP). ... The prevalence of CH was 12%. Some breeds had an increased RR of CH, although sample sizes were small. Dogs with CP had an increased RR of reactive hepatitis but no significant association with the other liver diseases. ... CH is common in the first opinion dog population but less common than CP. CP was significantly associated with reactive hepatitis but not CH. Possible breed associations mirrored another recent UK study. Some dogs with CP may be erroneously diagnosed clinically as having CH on the basis of increased serum liver enzymes because of concurrent reactive hepatitis if the diagnosis is not confirmed histologically."
Observational study of 14 cases of chronic pancreatitis in dogs. P. J. Watson, J. Archer, A. J. Roulois, T. J. Scase, M. E. Herrtage. Vet. Rec. Dec. 2010;167(25):968-976. Quote: "This study reports the clinical, clinicopathological and ultrasonographic findings from dogs with chronic pancreatitis (CP). Fourteen dogs with clinical signs consistent with CP and histological confirmation of the disease were evaluated. ... (...two Cavalier King Charles spaniels). ... Spaniels were the most common breed with CP, representing seven of the 14 dogs in this study. ... ...with Cavalier King Charles and cocker spaniels having a perilobular pattern, while other breeds had an intralobular distribution... There were a large number of spaniels in the current study, mirroring a pathology study (Watson and others 2007) that found an increased relative risk of pancreatitis in Cavalier King Charles and cocker spaniels, providing further evidence for breed-related disease in spaniels. ...CP was histologically severe in nine cases. Most dogs showed chronic low-grade gastrointestinal signs and abdominal pain. Five dogs had exocrine pancreatic insufficiency and five dogs had diabetes mellitus. The sensitivity of elevated trypsin-like immunoreactivity for CP was 17 per cent. The sensitivities of canine pancreatic lipase immunoreactivity, lipase and amylase for CP were 44 to 67 per cent or 14 to 28 per cent depending on the cut-off value used. Cholesterol was elevated in 58 per cent of samples. Liver enzymes were often elevated. The pancreas appeared abnormal on 56 per cent of ultrasound examinations. Ten dogs had died by the end of the study period; only one case was due to CP. CHRONIC pancreatitis (CP) in dogs is poorly documented clinically. However, a recent study reported the prevalence of CP to be 34 per cent in postmortem examinations of dogs from first opinion practice ... ."
Exocrine Pancreatic Insufficiency in Dogs. Joseph Cyrus Parambeth and Jörg M. Steiner. Consultant on Call: Gastroenterology, NAVC Clinician’s Brief ; May 2011. Quote: "Chronic pancreatitis can result in destruction of acinar cells (all breeds are affected, but cavalier King Charles spaniels and Jack Russell terriers may be predisposed)."
Genetic Connection: A Guide to Health Problems in Purebred Dogs, Second Edition. Lowell Ackerman. July 2011; AAHA Press; pg 76. Quote: "... breed predispositions have been reported for chow chows and Cavalier King Charles spaniels."
Sensitivity and Specificity of Canine Pancreas-Specific Lipase (cPL) and Other Markers for Pancreatitis in 70 Dogs with and without Histopathologic Evidence of Pancreatitis. S. Trivedi, S.L. Marks, P.H. Kass, J.A. Luff, S.M. Keller, E.G. Johnson, B. Murphy. J Vety Int Med Nov/Dec 2011;25(6):1241-1247. Quote: "Pancreatitis is a common disorder in dogs for which the antemortem diagnosis remains challenging. Objectives: To compare the sensitivity and specificity of serum markers for pancreatitis in dogs with histopathologic evidence of pancreatitis or lack thereof. Animals: Seventy dogs necropsied for a variety of reasons in which the pancreas was removed within 4 hours of euthanasia and serological markers were evaluated within 24 hours of death. Methods: Prospective study: Serum was analyzed for amylase and lipase activities, and concentrations of canine trypsin-like immunoreactivity (cTLI) and canine pancreas-specific lipase (cPL). Serial transverse sections of the pancreas were made every 2 cm throughout the entire pancreas and reviewed using a semiquantitative histopathologic grading scheme. Results: The sensitivity for the Spec cPL (cutoff value 400 μg/L) was 21 and 71% in dogs with mild (n = 56) or moderate-severe pancreatitis (n = 7), and 43 and 71% (cutoff value 200 μg/L), respectively. The sensitivity for the cTLI, serum amylase, and lipase in dogs with mild or moderate-severe pancreatitis was 30 and 29%; 7 and 14%; and 54 and 71%, respectively. The specificity for the Spec cPL based on 7 normal pancreata was 100 and 86% (cutoff value 400 and 200 μg/L, respectively), whereas the specificity for the cTLI, serum amylase, and lipase activity was 100, 100, and 43%, respectively. Conclusion and Clinical Importance: The Spec cPL demonstrated the best overall performance characteristics (sensitivity and specificity) compared to other serum markers for diagnosing histopathologic lesions of pancreatitis in dogs."
Chronic Pancreatitis in Dogs. Penny Watson. Topics in Compan An Med August 2012;27(3):133-139. Quote: "Chronic pancreatitis used to be considered uncommon in dogs, but recent pathological and clinical studies have confirmed that it is in fact a common and clinically significant disease. Clinical signs can vary from low-grade recurrent gastrointestinal signs to acute exacerbations that are indistinguishable from classical acute pancreatitis. Chronic pancreatitis is a significant cause of chronic pain in dogs, which must not be underestimated. It also results in progressive impairment of endocrine and exocrine function and the eventual development of diabetes mellitus or exocrine pancreatic insufficiency or both in some affected dogs at end stage. The etiology is unknown in most cases. Chronic pancreatitis shows an increased prevalence in certain breeds, and recent work in English Cocker Spaniels suggests it is part of a polysystemic immune-mediated disease in this breed. Breeds showing increased risk of chronic pancreatitis in the United Kingdom: Cavalier King Charles Spaniels, English Cocker Spaniels, Boxers, Collies. ... Cavalier King Charles Spaniels (CKCS) appear to show less obvious clinical signs and diagnostic imaging findings than other breeds, suggesting their disease is less inflammatory. ... CKCSs show a predominance of periductular and perivascular fibrosis and ductular hyperplasia. ... The histological and clinical appearance is different in different breeds, suggesting that etiologies may also be different. Diagnosis is challenging because the sensitivities of the available noninvasive tests are relatively low. However, with an increased index of suspicion, clinicians will recognize more cases that will allow them to institute supportive treatment to improve the quality of life of the patient. ... The author would have a high index of suspicion that DM [diabetes mellitus] in any older dog of a breed predisposed to CP [chronic pancreatitis] such as Cocker Spaniel or CKCS may in fact be caused by CP. ... The occurrence of DM or EPI [exocrine pancreatic insufficiency] in an older ECS [English Cocker spaniels] or CKCS greatly increases the index of suspicion for underlying CP.
Current Status of Genetic Studies of Exocrine Pancreatic Insufficiency in Dogs. Leigh Anne Clark. Topics in Comp. Anim.Med. May 2012. Quote: "Exocrine pancreatic insufficiency (EPI) is a disorder wherein the pancreas fails to secrete adequate amounts of digestive enzymes. In dogs, EPI is usually the consequence of an autoimmune disease known as pancreatic acinar atrophy. Originally believed to be a simple autosomal recessive disorder, a test-breeding recently revealed that EPI has a more complex mode of inheritance. The contributions of multiple genes, combined with environmental factors, may explain observed variability in clinical presentation and progression of this disease. Research efforts aim to identify genetic variations underlying EPI to assist breeders in their efforts to eliminate this disease from their breed and provide clinicians with new targets for therapeutic intervention and/or disease prevention. Genome-wide linkage, global gene expression, and candidate gene analyses have failed to identify a major locus or genetic variations in German Shepherd Dogs with EPI. Recently, genome-wide association studies revealed numerous genomic regions associated with EPI. Current studies are focused on alleles of the canine major histocompatibility complex. In this article we review findings from scientific investigations into the inheritance and genetic cause(s) of EPI in the purebred dog."
Exocrine Pancreatic Insufficiency in the Dog: Breed Associations, Nutritional Considerations, and Long-term Outcome. Alexander J. German. Topics in Comp. Anim.Med. May 2012. Quote: "Canine exocrine pancreatic insufficiency (EPI) is an alimentary tract disorder causing malabsorption and debilitations in affected individuals. This article covers predisposing factors to EPI and response to therapy. ... EPI is most commonly found in German Shepherds, followed by Rough-coated Collies, Chow Chows, and Cavalier King Charles Spaniels. ... Although relatively easy to diagnose, knowledge of breed predispositions (and also of those breeds where the disease is less common) can guide the clinician. Numerous studies have examined therapy for EPI, and a key finding is the variability in response among affected dogs. This implies that close monitoring and individual tailoring of therapy is needed to maximize the chance of success. Important factors affecting outcome are the choice of enzyme preparation, presence of hypocobalaminemia, and the response to the first 2 to 3 months of therapy."
Pathophysiology of Acute Pancreatitis: Potential Application from Experimental Models and Human Medicine to Dogs. Caroline Mansfield. J.Vet.Intern.Med. July 2012; 26(4):875-887. Quote: "The cellular events leading to pancreatitis have been studied extensively in experimental models. Understanding the cellular events and inciting causes of the multisystem inflammatory cascades that are activated with this disease is of vital importance to advance diagnosis and treatment of this condition. Unfortunately, the pathophysiology of pancreatitis in dogs is not well understood, and extrapolation from experimental and human medicine is necessary. The interplay of the inflammatory cascades (kinin, complement, cytokine) is extremely complex in both initiating leukocyte migration and perpetuating disease. Recently, nitric oxide (NO) and altered microcirculation of the pancreas have been proposed as major initiators of inflammation. In addition, the role of the gut is becoming increasingly explored as a cause of oxidative stress and potentiation of systemic inflammation in pancreatitis."
A Multi-Institutional Study Evaluating the Diagnostic Utility of the Spec cPL™ and SNAP® cPL™ in Clinical Acute Pancreatitis in 84 Dogs. K. McCord, P.S. Morley, J. Armstrong, K. Simpson, M. Rishniw, M.A. Forman, D. Biller N. Parnell, K. Arnell, S. Hill, S. Avgeris, H. Gittelman, M. Moore, M. Hitt, G. Oswald, S. Marks, D. Burney, D. Twedt. J.Vet.Intern.Med. July 2012; 26(4):888-896. Quote: "Background: Pancreas-specific lipase is reported to aid in diagnosing acute pancreatitis (AP) in dogs but has not been rigorously evaluated clinically. Hypothesis/Objectives: To describe variability of disease in dogs with suspected clinical AP, and to evaluate accuracy of 2 pancreatic-specific lipase immunoassays, Spec cPL (SPEC) and SNAP cPL (SNAP), in diagnosing clinical AP. We hypothesized that SPEC and SNAP provide better diagnostic accuracy than serum amylase or total lipase. Animals: A total of 84 dogs; 27 without AP and 57 with clinical signs associated with AP. Methods: Multicenter study. Dogs were prospectively enrolled based upon initial history and physical examination, then retrospectively classified into groups according to the likelihood of having clinical AP by a consensus of experts blinded to SPEC and SNAP results. Bayesian latent class analyses were used to estimate the diagnostic accuracy of SPEC and SNAP. Results: The estimates for test sensitivities and specificities, respectively, ranged between 91.5–94.1% and 71.1–77.5% for SNAP, 86.5–93.6% and 66.3–77.0% for SPEC (cutoff value of 200 μg/L), 71.7–77.8% and 80.5–88.0% for SPEC (cutoff value of 400 μg/L), and were 52.4–56.0% and 76.7–80.6% for amylase, and 43.4–53.6% and 89.3–92.5% for lipase. Conclusions and Clinical Importance: SNAP and SPEC have higher sensitivity for diagnosing clinical AP than does measurement of serum amylase or lipase activity. A positive SPEC or SNAP has a good positive predictive value (PPV) in populations likely to have AP and a good negative predictive value (NPV) when there is low prevalence of disease." Note: SPEC and SNAP are IDEXX products. IDEXX sponsored the study.
A blinded randomised controlled trial to determine the effect of enteric coating on enzyme treatment for canine exocrine pancreatic insufficiency. Aran Mas, Peter-John M Noble, Peter J Cripps, Daniel J Batchelor, Peter Graham, Alexander J German. BMC Vet. Res. July 2012;8:127. Quote: "Background: Enzyme treatment is the mainstay for management of exocrine pancreatic insufficiency (EPI) in dogs. ‘Enteric-coated’ preparations have been developed to protect the enzyme from degradation in the stomach, but their efficacy has not been critically evaluated. The hypothesis of the current study was that enteric coating would have no effect on the efficacy of pancreatic enzyme treatment for dogs with EPI. Thirty-eight client-owned dogs with naturally occurring EPI (including 1 cavalier King Charles spaniel) were included in this multicentre, blinded, randomised controlled trial. Dogs received either an enteric-coated enzyme preparation (test treatment) or an identical preparation without the enteric coating (control treatment) over a period of 56 days. Results: There were no significant differences in either signalment or cobalamin status (where cobalamin deficient or not) between the dogs on the test and control treatments. Body weight and body condition score increased in both groups during the trial (P<0.001) but the magnitude of increase was greater for the test treatment compared with the control treatment (P<0.001). By day 56, mean body weight increase was 17% (95% confidence interval 11-23%) in the test treatment group and 9% (95% confidence interval 4-15%) in the control treatment group. The dose of enzyme required increased over time (P<0.001) but there was no significant difference between treatments at any time point (P=0.225). Clinical disease severity score decreased over time for both groups (P=0.011) and no difference was noted between groups (P=0.869). No significant adverse effects were reported, for either treatment, for the duration of the trial. Conclusions: Enteric coating a pancreatic enzyme treatment improves response in canine EPI. ... VetPlus Ltd., who markets the product on which both treatments were based, funded the trial."
Chronic pancreatitis in dogs: A retrospective study of clinical, clinicopathological, and histopathological findings in 61 cases. Brier M. Bostrom, Panagiotis G. Xenoulis, Shelley J. Newman, Roy R. Pool, Geoffrey T. Fosgate, Jörg M. Steiner. Vet.J. Jan 2013; 195(1):73-79. Quote: "The objective of this study was to characterize the clinical, clinicopathological, and histopathological findings of dogs with chronic pancreatitis. The necropsy database at Texas A&M University was searched for reports of dogs with histological evidence of chronic pancreatitis defined as irreversible histologic changes of the pancreas (i.e. fibrosis or atrophy). A reference necropsy population of 100 randomly selected dogs was used for signalment and concurrent disease comparisons. Cases were categorized as clinical or incidental chronic pancreatitis based on the presence of vomiting, decreased appetite, or both vs. neither of these signs. All archived pancreas samples were scored histologically using a published scoring system. Sixty-one dogs with chronic pancreatitis were included ... mainly English Cocker Spaniels and Cavalier King Charles Spaniels. ... The most frequent clinical signs were lethargy, decreased appetite, vomiting, and diarrhea. Compared to the reference necropsy population, chronic pancreatitis cases were more likely to be older, neutered, of the non-sporting/toy breed group, and to have concurrent endocrine, hepatobiliary, or neurological disease. Clinical cases had significantly higher histological scores for pancreatic necrosis and peripancreatic fat necrosis, and were significantly more likely to have hepatobiliary or endocrine disease as well as increased liver enzyme activities, or elevated cholesterol and bilirubin concentrations. In conclusion, clinical disease resulting from chronic pancreatitis might be related to the presence of pancreatic necrosis and pancreatic fat necrosis. The signalment, presentation, and concurrent diseases of dogs with chronic pancreatitis are similar to those previously reported for dogs with acute pancreatitis."
Haemolytic anaemia and acute pancreatitis associated with zinc toxicosis in a dog. R. Blundell, F. Adam. Vety. Rec. July 2013;doi: 10.1136/vetreccr.100376rep. Quote: "We describe a case of zinc toxicity in a 14-month-old, female, neutered, Cavalier King Charles spaniel with a 48-hour history of haematochezia, icterus and collapse. Regenerative anaemia with a packed-cell volume of 7 per cent was seen. Prior to referral, radiography had revealed a gastric, metallic foreign body which was removed at exploratory laparotomy. On presentation, the dog was comatose, hypothermic and bradycardic – resuscitation was performed successfully, but the dog then displayed marked abdominal pain. The dog died 12 hours after presentation. At postmortem examination, the animal showed severe icterus. Both kidneys were diffusely dark red; the pancreas was diffusely pale and nodular. Histopathological examination revealed evidence of intravascular haemolysis with blood vessel lumens containing haemoglobin. The renal tubules also contained large amounts of intraluminal haemoglobin with haemoglobin crystals scattered throughout the cortex and medulla. The pancreas exhibited multifocal coagulative necrosis, surrounded by a neutrophil-dominated inflammatory infiltrate. Zinc levels were markedly increased above the normal reference range in both liver and kidney. This report describes the clinical and pathological findings of a case of acute zinc toxicity in a dog following ingestion of a metallic object which resulted in marked haemolytic anaemia and acute pancreatitis."
Clinical Forum: canine pancreatitis and biliary duct obstruction. Irene Schaafsma, Kate Bradley, Andrew Denning, Esther Barett. Companion Anim. June 2013;18(4):147-150. Quote: "Part 2: The radiologist's perspective: This clinical forum will review pancreatic disease in dogs, primarily focusing on those patients that go on to develop obstruction of the biliary tree. A series of commonly asked questions relating to pancreatitis and concurrent biliary tract obstruction will be asked of a panel of specialists with varying views expressed! ... Some breeds are predisposed, including Cavalier King Charles Spaniels, English Cocker Spaniels, Miniature Schnauzers and Boxers. ... In the August 2013 issue of Companion Animal, a further article on this topic will be published giving both a surgeon's perspective on canine pancreatitis and biliary duct obstruction."
Canine Pancreatitis. Andrew Linklater. Clinician's Brief. October 2013.
Nutritional management of acute pancreatitis in dogs and cats. Kristine B. Jensen, Daniel L. Chan. J.Vet. Emergency & Critical Care. May 2014;24(3):240-250. Quote: "Objective: To review current and emerging nutritional approaches in the management of acute pancreatitis (AP) in people, dogs, and cats, and to provide a framework for further investigation in this field. Summary: Nutritional management is an important part of the treatment plan for patients with AP. In human medicine, the general approach for providing nutrition in patients with AP has changed in recent years and favors enteral over parenteral nutrition with an emphasis on early enteral nutrition (EN). Although there are limited data available, there is increasing evidence in the veterinary literature that supports the beneficial role of EN in AP and contradicts previous assumptions about poor tolerance to enteral feeding in this patient population. Parenteral nutrition may be appropriate alone or in combination with EN as a temporary measure in malnourished patients that do not tolerate adequate EN; however, enteral feeding should be attempted first in most cases. Immunonutrition is being investigated for its positive role in modulating pancreatic inflammation and improving gut barrier function in cases of human AP. Conclusions: The nutritional management of veterinary patients with AP remains challenging. Based on clinical evidence in people, experimental animal studies, and preliminary studies in dogs and cats, the choice of EN over parenteral nutritional support during AP in dogs and cats appears to be beneficial and well tolerated. Optimization of nutritional therapies in dogs and cats including the use of immunonutrition during AP warrants further investigation."Pancreatitis in Cavaliers: What is it and what can I do about it? Penny Watson. Companion Cavalier Club Health Seminar. November 2014.DVD. Quote: "So the cavalier disease, we've been very lucky ... to be able to look at sections of pancreas now of over 40 cavalier King Charles spaniels, most of which were older but some of which were younger. So, we have an age range. ... What we've found, just looking at the histology, is that there is a very high prevalence, and that by the time we get to dogs of 11, 12, 13, I would be surprised to see a normal pancreas. And I would say the prevalence of chronic pancreatitis in cavaliers mimics mitral valve disease. ... I would say about 80%. ... Like mitral valve disease, it is a disease of aging. It is not so common in younger dogs. ... We had a theory that these dogs have an increased propensity to produce scar tissue, and that in fact they are doing it in multiple organs. So, there is so link between some of these diseases. ... When we look at the central nervous system in dogs with syringomyelia histologically, we find more fibrosis around blood vessels than you would normally find in a normal dog. ... We don't know what's causing the scarring in the pancreas. There is something causing it, and it seems to be coming up the ducts because that's where a lot of this is happening. And actually my theory at the moment is that it has something to do with the duct bacteria. And that theory has developed after seeing not one or two, but actually four or five cavaliers with chronic pancreatitis who respond very well to antibiotic therapy, metronidazole therapy specifically. And that's the sort of antibiotic that we use for overgrowth of bacteria in the small intestine, not the sort of antibiotic we use for other infections. And so I either think they've got gut bacteria coming up the duct, and perhaps their normal gut bacteria and it just that cavaliers' over-responding. Or, maybe there's something about their duct flora that's driving it, but I think there is a link there, somehow or another between the cavalier's gut flora and what's happening in the pancreas. Now why might they [cavaliers] be forming too much scar tissue? ... A current theory revolves around their platelets. Platelets are blood clotting cells. ... In cavaliers, about 50% of cavaliers in the UK have these macro-platelets, these jumbo platelets. ... Something in these cavaliers is stimulating these stellate cells to transform and produce lots of fibrous tissue. ... We noticed in cavaliers ... that there was a pattern of increased fibrosis in multiple organs, the kidneys particularly. Mitral valve disease isn't scarring. Mitral valve disease is myxomatous change. ... But the cells that produce that are valvular interstitial cells, and they are identical to the stellate cells in the pancreas. The current theory ... is that these little dogs might have something in their platelets that they are releasing when they are going through blood vessels into different organs that's tending to cause fibrosis. And our theory ... is that this might be serotonin, which is also known as 5-hydroxytryptamine, because platelets contain a bucket load of serotonin. ... We already know that some cavaliers have elevated levels of serotonin, that's been shown. We also already know that serotonin is central to converting those valvular interstitial cells into myofibroblasts. ... I think what was most compelling for me was the human side of it. There is a particular horrible syndrome in people called carcinoid syndrome. People who've got serotonin secreting tumors that they've got. ... They get pancreatic, liver, and kidney fibrosis and mitral valve disease. ... So in a nutshell, the hypothesis was these big floppy platelets release serotonin easily as they pass through vessels, leading to fibrosis in perivascular areas."
Pancreatitis in dogs and cats: definitions and pathophysiology. P. Watson. J. Sm. Anim. Pract. January 2015;56(1):3-12. Quote: Pancreatitis, or inflammation of the pancreas, is commonly seen in dogs and cats and presents a spectrum of disease severities from acute to chronic and mild to severe. It is usually sterile, but the causes and pathophysiology remain poorly understood. The acute end of the disease spectrum is associated with a high mortality but the potential for complete recovery of organ structure and function if the animal survives. At the other end of the spectrum, chronic pancreatitis in either species can cause refractory pain and reduce quality of life. It may also result in progressive exocrine and endocrine functional impairment. There is confusion in the veterinary literature about definitions of acute and chronic pancreatitis and there are very few studies on the pathophysiology of naturally occurring pancreatitis in dogs and cats. This article reviews histological and clinical definitions and current understanding of the pathophysiology and causes in small animals by comparison with the much more extensive literature in humans, and suggests many areas that need further study in dogs and cats. ... Dogs with EPI as a result of end-stage CP tend to be middle-aged to older medium- or small-breed dogs, particularly Cavalier King Charles spaniels (CKCS), English cocker spaniels, and Border collies. One study reported an increased prevalence of EPI in older CKCS and, although the aetiology was unknown, end stage CP was suggested because of the older age at presentation of these dogs. ... There is confusion in the veterinary literature about definitions of acute and chronic pancreatitis and there are very few studies on the pathophysiology of naturally occurring pancreatitis in dogs and cats. This article reviews histological and clinical definitions and current understanding of the pathophysiology and causes in small animals by comparison with the much more extensive literature in humans, and suggests many areas that need further study in dogs and cats.
Diagnosis of pancreatitis in dogs and cats. P. G. Xenoulis. J. Small Animal Practice. January 2015;56(1):13-26. Quote: "Pancreatitis is the most common disorder of the exocrine pancreas in both dogs and cats. ... Cocker spaniels, Cavalier King Charles spaniels, Border collies and boxers have been reported to be at increased risk for chronic pancreatitis in the UK (Watson et al. 2007). ... Ante-mortem diagnosis of canine and feline pancreatitis can be challenging. The clinical picture of dogs and cats with pancreatitis varies greatly (from very mild to severe or even fatal) and is characterised by non-specific findings. Complete blood count, serum biochemistry profile and urinalysis should always be performed in dogs and cats suspected of having pancreatitis, although findings are not-specific for pancreatitis. Serum amylase and lipase activities and trypsin-like immunoreactivity (TLI) concentrations have no or only limited clinical value for the diagnosis of pancreatitis in either dogs or cats. Conversely, serum pancreatic lipase immunoreactivity (PLI) concentration is currently considered to be the clinicopathological test of choice for the diagnosis of canine and feline pancreatitis. Abdominal radiography is a useful diagnostic tool for the exclusion of other diseases that may cause similar clinical signs to those of pancreatitis. Abdominal ultrasonography can be very useful for the diagnosis of pancreatitis, but this depends largely on the clinician's experience. Histopathological examination of the pancreas is considered the gold standard for the diagnosis and classification of pancreatitis, but it is not without limitations. In clinical practice, a combination of careful evaluation of the animal's history, serum PLI concentration and abdominal ultrasonography, together with pancreatic cytology or histopathology when indicated or possible, is considered to be the most practical and reliable means for an accurate diagnosis or exclusion of pancreatitis compared with other diagnostic modalities."
Management of acute pancreatitis in dogs: a critical appraisal with focus on feeding and analgesia. C. Mansfield, T. Beths. J. Small Animal Practice. January 2015;56(1):27-39. Quote: "Knowledge about acute pancreatitis has increased recently in both the medical and veterinary fields. Despite this expansion of knowledge, there are very few studies on treatment interventions in naturally occurring disease in dogs. As a result, treatment recommendations are largely extrapolated from experimental rodent models or general critical care principles. General treatment principles involve replacing fluid losses, maintaining hydrostatic pressure, controlling nausea and providing pain relief. Specific interventions recently advocated in human medicine include the use of neurokinin-1 antagonists for analgesia and early interventional feeding. The premise for early feeding is to improve the health of the intestinal tract, as unhealthy enterocytes are thought to perpetuate systemic inflammation. The evidence for early interventional feeding is not supported by robust clinical trials to date, but in humans there is evidence that it reduces hospitalisation time and in dogs it is well tolerated. This article summarises the major areas of management of acute pancreatitis in dogs and examines the level of evidence for each recommendation."
Diabetes mellitus and pancreatitis – cause or effect? L. J. Davison. J. Small Animal Practice. January 2015;56(1):50-59. Quote: "Diabetes mellitus and pancreatitis are two distinct diseases encountered commonly in small animal practice. Whilst the clinical signs of diabetes mellitus are usually unmistakeable, a firm diagnosis of pancreatitis can prove more elusive, as clinical signs are often variable. ... Recent work to examine the breed-related prevalence of CP in postmortem pancreata from first opinion practice in the UK suggested that histological evidence of CP in dogs is present in approximately 34% of cadavers, with Cavalier King Charles spaniels (CKCS), collies and boxers being over-represented (Watson et al. 2007). ... Over the past 10 to 15 years, despite the fact that the clinical signs of diabetes mellitus are remarkably consistent, it has become more apparent that the underlying pathology of diabetes mellitus in dogs and cats is heterogeneous, with exocrine pancreatic inflammation accompanying diabetes mellitus in a number of cases. However, the question remains as to whether the diabetes mellitus causes the pancreatitis or whether, conversely, the pancreatitis leads to diabetes mellitus – as there is evidence to support both scenarios. The concurrence of diabetes mellitus and pancreatitis has clinical implications for case management as such cases may follow a more difficult clinical course, with their glycaemic control being “brittle” as a result of variation in the degree of pancreatic inflammation. Problems may also arise if abdominal pain or vomiting lead to anorexia. In addition, diabetic cases with pancreatitis are at risk of developing exocrine pancreatic insufficiency in the following months to years, which can complicate their management further."
Canine Pancreatic-Specific Lipase Concentrations in Dogs with Heart Failure and Chronic Mitral Valvular Insufficiency. D. Han, R. Choi, C. Hyun. J. Vet. Internal Medicine. January 2015;29(1);180-183. Quote: "Background: Chronic mitral valvular insufficiency (CMVI) in dogs is very common and might cause clinical signs of congestion and poor tissue perfusion. Hypothesis: Poor tissue perfusion from CMVI causes pancreatitis in dogs, as indicated by serum pancreatic lipase concentrations. Animals: Sixty-two client-owned dogs consisting of 40 dogs [none were cavalier King Charles spaniels] with different stages of heart failure from CMVI and 22 age-matched healthy dogs, based on full cardiac exam and routine laboratory tests. Methods: Prospective, controlled, observational study. Serum canine pancreatic lipase immunoreactivity (cPLI) concentrations were determined by quantitative cPLI test in healthy and CMVI groups. Results: Serum cPLI concentrations were 54.0 μg/L (IQR: 38.0–78.8 μg/L) in control, 55.0 μg/L (IQR: 38.3–88.8 μg/L) in ISACHC I, 115.0 μg/L (IQR: 45.0–179.0 μg/L) in ISACHC II and 223.0 μg/L (IQR: 119.5–817.5 μg/L) in ISACHC III. Close correlation to serum cPLI concentration was found in the left atrial to aorta (LA/Ao) ratio (r = 0.597; P = .000) and the severity of heart failure (r = 0.530; P = .000). Conclusions and Clinical Importance: ... This study clearly found the increase in cPL in dogs with advanced heart failure, suggesting that the risk of pancreatitis might be increased with the worsening of heart failure signs in dogs. ... This study found CMVI is associated with pancreatic injury in congestive heart failure caused by CMVI. ... There were several limitations to this study. First, the study population was small and may not have provided sufficient statistical power to adequately reflect the correlation of cPLI to the severity of heart failure in CMVI dogs. Second, the influence on renal dysfunction by cardiac medication and/or heart failure was not assessed in our study population and diminished renal clearance can cause the increase in cPLI in dog with more advanced stage of heart failure. Thirdly, many dogs diagnosed as pancreatitis by cPLI test have never been confirmed by the histopathological exam, although the diagnostic value of the cPLI on pancreatitis has been clearly proven in dogs.[13, 14] Fourthly, the dogs showing subclinical pancreatitis were not more carefully assessed for malassimilation, yet maldigestion and malabsorption are known to occur in dogs with advanced stages of heart failure.[18] Finally, we did not demonstrate the presence of gastrointestinal findings with increased serum PLI concentrations, thereby weakening any conclusions that clinical pancreatitis may arise as a complication of heart failure in dogs with CMVI. Despite these study limitations, our study results clearly suggest that the increased serum PLI concentration, to levels accepted as indicating pancreatitis, is a common comorbidity with congestive heart failure. Therefore, regular check-up for serum PLI level is warranted for early detection of pancreatitis from chronic heart diseases."
Effects of castration on cortisol and serotonin levels in dogs: Correlations between hormones and behavior. Elin Larsson. Swedish Univ. of Ag. Sciences. February 2015. Quote: "How behavior in dogs is affected by castration is unclear but there are increasing numbers of castrated dogs in Sweden and a common reason for castration is the owner hoping for behavioral problems to decrease. To study if the concentrations of behaviorally associated hormones are changing after castration and if the changes correlates with alteration in behavior may contribute to more knowledge about how castration affect dogs. In this study, seven bitches and three male dogs [including a male cavalier King Charles spaniel] were studied before and until four weeks after castration by analyzing cortisol and serotonin levels in urinary samples and through behavioral questionnaires to the dog owners. Cortisol is an important stress hormone and the serotonin system is largely involved in mental well-being. Creatinine was also analyzed in purpose of calculating hormone levels as hormone and creatinine concentration ratios, to minimize urinary density affecting the hormone levels. The females had significantly lower cortisol levels after castration than before. Among the bitches, the serotonin levels tended to increase after castration. The male dogs were few in number and no obvious changes in hormone levels were shown. It was not possible to see any clear behavioral changes but the bitches showed tendencies to be more active, more playful and more willing to be close to their owners. In order to draw reliable conclusions about effects of castration on hormone levels in dogs and if there is connection with any changes in behavior, more studies with larger numbers of dogs and more detailed behavioral studies are needed. It would also be interesting to study hormone levels and behavior during a longer period of time after castration."
DGGR is not a specific substrate for pancreatic lipase. J. M. Steiner, J. S. Suchodolski, R. Gomez. Proceedings of the 2015 WSAVA World Congress. May 2015. Quote: Serum lipase activity in dogs can be measured by different types of assays. Most assays utilize a 1,2-diglyceride as a substrate, others triolein, and yet others DGGR. This latter substrate has been utilized in human medicine for more than 20 years. However, recently some reports have suggested that DGGR-based assays are specific for measurement of pancreatic lipase in dog serum. Dogs with exocine pancreatic insufficiency (EPI) are considered to have lost moe than 90% of their secretory capacity. Thus, the aim of this study was to measure serum lipase activity by a DGGR-based assay in dogs with EPI and compare them to serum lipase activities in healthy dogs. Leftover serum samples from 48 dogs with a serum cTLI concentration ≤ 1.0 µg/L were selected. Serum samples from 66 healthy dogs were used as controls. Serum lipase activity was measured by a DGGR-based assay and was compared between dogs with EPI and healthy control dogs. The number of dogs with EPI with a serum lipase activity within hte reference interval was determined. Serum lipase activitty was significantly lower in dogs with EPI (median: 34U/L; range 20-94 U/L) than that in healthy control dogs (median: 74 U/L; range 23-308 U/L;p-value: <0.0001). However, 33/48 EPI dogs (69%) had serum lipase activities within the reference interval (31-174 U/L), suggesting that DGGR is not exclusively hydrolyzed by pancreatic lipase and DGGR-based assays are thus not specific for this enzyme. Which other lipases are detected by DGGR-bsed assays remains to be determined.
Canine pancreas-specific lipase (spec cPL) and C-reactive protein (CRP) in dogs treated with anticonvulsants (phenobarbital and potassium bromide). Viviana Albarracín, Mariana Teles, Antonio Meléndez-Lazo, Jaume Rodón, Josep Pastor. Topics in Companion Animal Med. July 2015. Quote: "Animals treated with anticonvulsant drugs may have increased canine pancreas-specific lipase values. Inflammatory conditions and specifically acute pancreatitis is of major concern in these animals. Elevation in C-reactive protein is being associated with inflammatory status in dogs and it has been correlated with the clinical severity of pancreatitis. In the present study, we investigated if there is a correlation between the canine pancreas-specific lipase increase, changes in C-reactive protein and hepatic enzymes, as well as, the incidence of severe acute pancreatitis in dogs with anticonvulsant treatment (phenobarbital, and/or potassium bromide). Increased values of pancreas-specific lipase were found in 6.8% of the animals in treatment with anticonvulsants, and this increase is correlated with the increase in triglycerides, alkaline phosphatase and alanine aminotransferase but not with C-reactive protein levels which suggest a possible induction/release phenomenon rather than a clear severe acute pancreatitis. C-reactive protein levels did not affect canine pancreas-specific lipase values on the population studied. Only two animals had clinical and analytical data suggested of acute pancreatitis, indicating a low prevalence (0.6%). In conclusion, canine pancreas-specific lipase may be increased in a low percentage of animals with anticonvulsants treatment and its increase may not be associated with severe acute pancreatitis. May be it is induced by the anticonvulsants drugs however, further studies are advised to rule out other possible causes that increased canine pancreas-specific lipase."
Clinical Utility of Diagnostic Laboratory Tests in Dogs with Acute Pancreatitis: A Retrospective Investigation in a Primary Care Hospital. M. Yuki, T. Hirano, N. Nagata, S. Kitano, K. Imataka, R. Tawada, R. Shimada, M. Ogawa. J. Vet. Intern. Med. November 2015. Quote: "Background: Acute pancreatitis (AP) occurs frequently in dogs, but most previous studies examining the diagnosis of AP have used data from secondary care hospitals. Hypothesis/Objectives: The aim of this study was to investigate the clinical utility of diagnostic laboratory tests in dogs with AP in a primary care hospital. Animals: Sixty-four dogs with clinical signs suggestive of AP diagnosed with nonpancreatic disease (NP) or AP. Methods: Medical records were retrospectively reviewed, including diagnostic laboratory tests considered potentially useful in the diagnosis of AP. The diagnostic accuracy of amylase and FUJI DRI-CHEM lipase (FDC lip) were investigated using receiver operating characteristics (ROC). In addition, we verified whether diagnostic laboratory tests were useful for evaluating duration of hospitalization and as biomarkers for monitoring recovery. Results: Activities of amylase and FDC lip were significantly higher in the AP group than in the NP group (P = .001, P < .001, respectively). The sensitivity of FDP lip activity for diagnosing AP was 100% (95% confidence interval [CI], 87.7–100%); the specificity was 89.5% (95% CI, 66.9–98.7%). Area under the ROC curve for FDC lip activity was 0.98 (95% CI, 0.93–1). High alanine aminotransferase (ALT) activity was associated with extended duration of hospitalization (P = .04). A significant difference in C-reactive protein (CRP) concentration before and 5 days after treatment was found (P = .001). Conclusions and clinical importance: Measurement of FDC lip activity appears useful for diagnosing AP. High ALT activity might be associated with prolonged duration of hospitalization, and CRP might be useful as a biomarker for monitoring recovery from AP."
Prevalence of pancreatic, hepatic and renal microscopic lesions in post-mortem samples from Cavalier King Charles Spaniels. Kent, Andrew C. C.; Constantino-Casas, Fernando; Rusbridge, Clare; Corcoran, Brendan; Carter, Margaret; Ledger, Tania; Watson, Penny J. J. Small Animal Practice. April 2016;57(4):188-193. Quote: "Objectives: To describe the prevalence of pancreatic, hepatic and renal microscopic lesions in post-mortem samples from [54] Cavalier King Charles Spaniels (CKCS) presented to a UK post-mortem collection scheme [The Cavalier Collection Scheme]. Methods: Histopathology was performed on the organs of interest and the prevalence of microscopic lesions described, this was related back to the clinical signs shown ante-mortem. Results: Evidence of chronic pancreatitis was seen in 51.9% of the cases, and age correlated with severity of disease, suggesting that chronic pancreatitis is a progressive condition. Evidence of renal lesions was present in 52.2% of cases, most commonly inflammatory disease. The rate of ante-mortem diagnosis was low for both pancreatic and renal disease, at 25% and 16.7% respectively. Primary hepatic lesions were present in only 11.1% of cases, but secondary hepatic lesions were more common and were present in 64.8%. Clinical Significance: Pancreatic and renal lesions are common in Cavalier King Charles Spaniels and clinicians should be aware of this when presented with clinical cases, they have similar rates of hepatic disease as the general population."
To Feed or Not to Feed? Controversies in the Nutritional Management of Pancreatitis. Justin Shmalberg. Today's Vet. Pract. November 2016. Quote: Small animals with pancreatitis should receive an assessment of their dietary history and nutritional status. Unfortunately, current knowledge is inadequate to provide a strong evidence-based recommendation on when and how to feed many patients. Dietary fat restriction appears to be a critical part of successful management of chronic disease in dogs, but its role in acute pancreatitis is less clear, and is generally unnecessary in cats. The definition of a low fat diet for patients with pancreatitis is not well established but may be less than 30 grams per 1000 kcal. Hyperlipidemic animals may benefit from restricted intake of fat to achieve lower serum triglycerides and cholesterol, but all animals require sufficient fat intake to ensure fat soluble vitamin absorption and to meet essential fatty acid requirements. When nutrition is elected for acute or severely affected patients, assistive feeding may be required. Current evidence suggests that enteral nutrition is preferred over parenteral nutrition unless there is a contraindication to luminal nutrition.
Method of Treating Canine Pancreatitis -- Camostat Mesilate. U.S. Patent Application 0170095440. Inventors: Long-Shiuh Chen, Diana Wood, Aidan Nuttall. Quote: A method for treating pancreatitis that involves identifying a patient with pancreatitis and administering to the patient a daily dose of Camostat Mesilate of between about 8 to about 1300 mg/kg or an equivalent amount of or 4-(4-guan-idino-benzoyloxy) phenylacetic acid is disclosed. The dosage can be administered as a single dose or can be administered in 2, 3, 4 or more doses to achieve the daily dose. The treatment can be given for a week (7 days), a month (31 days) or several months, or for as long as the treatment provides an increased quality of life. The drug can be administered orally in an oral capsule. The methods can be conveniently used in the treatment of canine pancreatitis by measuring the serum concentration of canine pancreas-specific lipase and administering a dose of the drug when the dog has a serum concentration of about 400 μg/L or more of canine pancreas-specific lipase. Example 1: Twenty-nine dogs with suspected chronic pancreatitis based on clinical signs and repeated measurements of an increased serum concentration of canine pancreas-specific lipase above a cut-off value for diagnosis of pancreatitis of about 400 μg/L or more received a dose of 4 or 8 mg/kg Camostat Mesilate q 8 hrs (12 or 24 mg/kg q d) over a period of 26±5 days. ... The treatment group treated with 4 mg/kg q 8 hrs Camostat Mesilate consisted of 1 intact female, 7 spayed females, and 4 neutered males with an average age [range] of 10.5 [2-14] years. The group treated with 8 mg/kg q 8 hrs Camostat Mesilate consisted of 4 intact females, 8 spayed females and 5 neutered males with an average age [range] of 11.5 [3-15] years. Overall, 20/29 dogs (70%) were 10 years or older and 15/29 dogs (52%) were spayed females. Dachshunds (n=6) and mixed breed dogs (n=6), followed by Miniature Schnauzers (n=3) and Cavalier King Charles Spaniels (n=2) were the most prominent breeds. ... Treatment of dogs with both dosages of Camostat Mesilate was only associated with very mild side effects, suggesting that this drug is generally safe for use in dogs. Also Camostat Mesilate administered orally at a dose of 24 mg/kg q d, led to a subjective improvement of quality of life in some patients based on reports from referring vets and pet owners. In addition, dogs in this study given an oral daily dose of 24 mg/kg showed a statistically significant decrease in serum concentrations of canine pancreas-specific lipase indicating attenuation of acinar cell damage. However, Camostat Mesilate did not lead to any significant changes in serum concentrations of C-reactive protein, S100A12, or TGF-β1, even though marked decreases were observed in individual patients.
Evaluation of SNAP cPL, Spec cPL, VetScan cPL Rapid Test, and Precision PSL Assays for the Diagnosis of Clinical Pancreatitis in Dogs. H. Cridge, A.G. MacLeod, G.E. Pachtinger, A.J. Mackin, A.M. Sullivant, J.M. Thomason , T.M. Archer, K.V. Lunsford, K. Rosenthal, R.W. Wills. J. Vet. Intern. Med. February 2018. DOI: 10.1111/jvim.15039. Quote: Background: The sensitivity, specificity, and agreement of 4 diagnostic assays (SNAP canine pancreatic lipase (cPL), specific cPL (Spec cPL), VetScan cPL Rapid Test, and Precision PSL) for pancreatitis in dogs have not been directly compared. Hypothesis/Objectives: To determine the level of agreement among each of the 4 assays and a clinical suspicion score, level of agreement among the assays, and sensitivity and specificity of each assay in a clinically relevant patient group. Animals: Fifty client-owned dogs [none were cavalier King Charles spaniels] with clinical signs of gastrointestinal disease. Methods: Prospective study. History, physical examination, complete blood count, serum biochemistry, abdominal ultrasound examination, and the 4 diagnostic assays for pancreatitis were performed. Intraclass correlation coefficients (ICC) were used to determine the level of agreement between each assay and a clinical suspicion score determined by a panel of 5 board-certified veterinary internists. Results: The ICC between the clinical suspicion score and the 4 assays were SNAP cPL, 0.61; Spec cPL, 0.68; VetScan cPL Rapid Test, 0.68; and Precision PSL, 0.60. The sensitivities of the assays ranged from 73.9 to 100.0%, whereas the specificities were SNAP cPL, 71.1–77.8%; Spec cPL, 74.1–81.1%; VetScan cPL Rapid Test, 76.9–83.8%; and Precision PSL, 64.0–74.3%. Conclusions and Clinical Importance: A good to excellent level of agreement was demonstrated among the 4 assays. ... Results of any of the 4 diagnostic assays alone, in the absence of supporting clinical findings, are insufficient to establish a diagnosis of clinical pancreatitis in dogs. ... The level of agreement among 4 currently available diagnostic assays for pancreatitis however was greater than the level of agreement between an individual diagnostic test and the clinical suspicion score. No single assay had high enough diagnostic specificity to conclusively diagnose pancreatitis based on a single test result, suggesting that a combination of signalment, physical examination, blood tests, a pancreatic lipase test, and ideally, abdominal ultrasound examination when available, may be the most practical means of establishing a definitive diagnosis of clinical pancreatitis in dogs.
Validation of a commercial 1,2-o-dilauryl-rac-glycero glutaric acid-(6’-methylresorufin) ester lipase assay for diagnosis of canine pancreatitis. Emily L Goodband, Gonçalo Serrano, Fernando Constantino-Casas, Joy Archer, Penny J Watson, Tim L Williams. Vet. Record. April 2018;5(1):doi:10.1136/vetreco-2017-000270. Quote: The objectives of this study were fourfold: technical validation of a commercial canine 1,2-o-dilauryl-rac-glycero glutaric acid-(6’-methylresorufin) ester (DGGR) lipase assay, to calculate a reference interval for DGGR lipase by the indirect a posteriori method, to establish biological validity of the assay, and to assess agreement between DGGR lipase and specific canine pancreatic lipase (Spec cPL) assays. Dogs with histologically confirmed acute pancreatitis (n=3), chronic pancreatitis (n=8) and normal pancreatic tissue (n=7) with stored (−80°C) serum samples were identified. Relevant controls were selected. Precision, reproducibility and linearity of DGGR lipase, and the effect of sample haemolysis and freezing, were assessed. Sensitivity and specificity of DGGR lipase and Spec cPL were determined. Agreement between these two parameters was calculated using Cohen’s kappa coefficient (κ). The DGGR lipase assay demonstrated excellent precision, reproducibility and linearity. Sample haemolysis and storage at −80°C for 12 months did not influence the assay. DGGR lipase (>245IU/l) and Spec cPL (>400µg/l) both showed poor sensitivity but excellent specificity for acute pancreatitis, and poor to moderate sensitivity but excellent specificity for chronic pancreatitis. Substantial agreement (κ=0.679) was found between DGGR lipase and Spec cPL. The validated DGGR lipase assay had similar sensitivity and specificity for the diagnosis of acute and chronic pancreatitis to Spec cPL. DGGR lipase is a reliable alternative to Spec cPL for the diagnosis of pancreatitis. ... DGGR has been considered to be more pancreas-specific than previously used lipase assays. However, a recent preliminary study found normal DGGR lipase activities in dogs with exocrine pancreatic insufficiency.15 This suggests DGGR may not be exclusively hydrolysed by pancreatic lipase; however, despite this, DGGR lipase was highly specific for pancreatitis in the present study. More studies are required to investigate these findings further, and DGGR is still likely to be more specific than the previously used 1,2-diglyceride assay.
Serum cobalamin and folate as prognostic factors in canine exocrine pancreatic insufficiency: An observational cohort study of 299 dogs. N. Soetart, D.Rochel, A. Drut, L.Jaillardon. Vet. J. January 2019;243(1):15-20. Quote: Exocrine pancreatic insufficiency (EPI) in dogs is a gastrointestinal condition leading to a severe impairment of nutrient absorption. The disease is frequently associated with vitamin disturbances especially regarding cobalamin and folate. Dogs with EPI need daily expensive supportive treatment. The aim of the present study was to identify prognostic factors for EPI in dogs, through a long-term survival study of 299 dogs, taking into account epidemiological, clinical, biological and therapeutic data, with particular emphasis on serum cobalamin and folate concentration. ... The three main breeds reported were German Shepherd dogs (GSD) (n = 139/290, 47.9%), Cavalier King Charles spaniels (CKCS) (20/290, 6.8%) and Rough coated collies (n = 10/290, 3.4%). ... CKCS dogs were significantly older at diagnosis (3.8, [0.3–14.8] years) than non-CKCS dogs, corroborating the fact that EPI is more likely due to end-stage chronic pancreatitis in this breed (6.5, [1.9–12.0] years) than other breeds. ... The prevalence of low serum cobalamin (cobalamin < 350 ng/L) and high serum folate (folate > 12 μg/L) concentrations were 67% (200/299) and 55% (164/299), respectively. Dogs with hypocobalaminemia at diagnosis were significantly older than those with serum cobalamin concentration within the reference interval (P < 0.001). Hypocobalaminemia at diagnosis (P = 0.04), male sex (P = 0.01), decreased appetite at diagnosis (P = 0.008) and not receiving enzyme replacement therapy (P = 0.003) were significant and independent risk factors for decreased survival in EPI. In contrast, hyperfolatemia was associated with improved prognosis (P = 0.02). These results confirm the importance of measuring serum cobalamin and folate concentrations at the time EPI is diagnosed, as hypocobalaminemia is negatively associated with prognosis, particularly in the absence of a high serum folate concentration.
Acute pancreatitis and acute kidney injury in dogs. E. Gori, I. Lippi, G. Guidi, F. Perondi, A. Pierini, V. Marchetti. Vet. J. March 2019;245:77-81. Quote: Acute pancreatitis and acute kidney injury are well-documented comorbidities in human medicine. Dogs that develop acute kidney injury during hospitalization have significantly higher mortality rates than those that do not. The aim of this study was to evaluate the prevalence of acute kidney injury in dogs with acute pancreatitis and the prognostic value of various clinicopathological parameters. Cases of acute pancreatitis presented between January 2012 and June 2016 were identified. The diagnosis of acute pancreatitis was based on two or more of the following clinical signs: abdominal pain, diarrhea, vomiting or anorexia/hyporexia, no other abdominal extra-pancreatic diseases at abdominal ultrasound, and abnormal SNAP cPL test. Diagnosis of acute kidney injury was based on the guidelines of the International Renal Interest Society. Dogs were classified into survivors and non-survivors. Serum creatinine, urea, amylase, total calcium, total cholesterol, C-reactive protein, WBC and band neutrophils were evaluated at admission. Clinical severity index was calculated at admission. Clinical and clinicopathological data were compared between survivors and non-survivors. Sixty-five dogs with acute pancreatitis [including two cavalier King Charles spaniels] were assessed. Clinical severity index ≥ 6.5 were associated with poor outcome (P = 0.0011). Serum urea and creatinine concentrations at admission were significantly lower in survivors than non-survivors (P < 0.0001 and P = 0.0002, respectively). Acute kidney injury was diagnosed in 17/65 dogs (26.2%) and was associated with poor outcome (P < 0.0001). Oligo-anuria was associated with poor outcome (P = 0.0294). Increased clinical severity index and azotemia in dogs with acute pancreatitis were associated with an increased risk of mortality. Acute kidney injury may be a comorbidity of canine acute pancreatitis. The presence of oligo-anuria is associated with poor outcome.
Correlation between NT-proBNP and lipase levels according to the severity of chronic mitral valve disease in dogs. Jun-Seok Park, Jae-Hong Park, Kyoung-Won Seo, Kun-Ho Song. J. Vet. Sci. July 2019;20(4):e43. Quote: Chronic mitral valve disease (CMVD) is the most common cardiovascular disease in dogs, causing decreased cardiac output that results in poor tissue perfusion and tissue damage to kidneys, pancreas, and other organs. The purpose of this study was to evaluate the relationships between heart disease severity and N-terminal pro B-type natriuretic peptide (NT-proBNP) and lipase in dogs with CMVD, as well as to evaluate longitudinal changes in these values. A total of 84 dogs participated in this 2015 to 2017 study. [None were cavalier King Charles spaniels.] Serum values of NT-proBNP and lipase were analyzed; radiography was used to measure the vertebral heart score and assess various echocardiographic values. NT-proBNP showed a strong positive correlation with increasing stage of heart disease; lipase showed a mild positive correlation with heart disease stage. When the three values (NT-proBNP, lipase and month) were continuously measured at 6-month intervals, all showed a correlation with the increasing length of the disease.
Advances in the diagnosis of acute pancreatitis in dogs. Harry Cridge, David C. Twedt, Angela J. Marolf, Leslie C. Sharkey, Jörg M. Steiner. J. Vet. Intern. Med. November 2021; doi: 10.1111/jvim.16292. Quote: In the last 20 years, the diagnosis of pancreatitis has become more frequent as a result of improved diagnostic modalities such as abdominal ultrasound examination, advanced imaging, and immunoassays for the measurement of pancreatic lipase. Our aim is to provide a state-of-the-art overview of the clinical diagnosis of acute pancreatitis (AP) in dogs with a particular focus on pancreatic lipase assay validation and clinical performance, in addition to advanced imaging modalities. We also discuss the potential indications for cytology and histopathology in dogs with suspected AP. Substantial advances have been made in the diagnostic approach to AP in dogs over the past several years, predominantly in the areas of diagnostic imaging and lipase assays.Weutilize a combination of suggestive clinical signs and physical examination findings, in conjunction with increased pancreatic lipase concentration and consistent findings on diagnostic imaging to make a clinical diagnosis of AP. Analytic validation is a prerequisite to clinical investigation when considering the use of lipase assays. Additionally, several diseases other than AP may result in increases in serum amylase or lipase activities. Although AUS frequently is used in the diagnosis of AP, the number of abnormalities detected likely influences test performance, with more abnormalities resulting in higher diagnostic specificity. Diseases other than AP also may result in similar ultrasonographic changes. It is likely that CTA and other advanced imaging modalities such as CEUS will play a larger role in the diagnosis of AP in dogs in the future. Given the lack of a single diagnostic gold standard and limited agreement between any single diagnostic modality and clinical reference standard, integration of clinical findings, imaging results, lipase assays, and cytologic or histopathologic findings, where available, will provide optimal diagnostic results. Enzyme activities or diagnostic imaging should not be utilized in isolation.
Prevalence of ultrasonographic gastrointestinal wall changes in dogs with acute pancreatitis: A retrospective study (2012-2020). Joshua J. Hardwick, Elizabeth J. Reeve, Melanie J. Hezzell, Jenny A. Reeve. J. Vet. Intern. Med. March 2022; doi: 10.1111/jvim.16414. Quote: Background: Ultrasonographic gastrointestinal wall changes in dogs with acute pancreatitis (AP) are not well characterized in the literature. No detailed studies have described their prevalence, characteristics, distribution, or clinical relevance. Hypothesis/Objectives: Describe the prevalence of ultrasonographic gastrointestinal wall changes in a population of dogs with AP and evaluate for associations between the presence of gastrointestinal wall changes and clinical or clinicopathological variables. Animals: Referral population of 66 client-owned dogs with AP. Methods: Retrospective search of clinical records to identify dogs with AP. Clinical variables, clinicopathological variables and ultrasonographic findings were reported using descriptive statistics. A binary logistic regression model was used to evaluate for associations between the presence of gastrointestinal wall changes and clinical or clinicopathological variables. Results: Sixty-six dogs were included. ... cavalier King Charles spaniel (n = 3) [4.545%] ... Forty-seven percent of dogs (95% confidence interval [CI], 35.0%-59.0%; n = 31) with AP had ultrasonographic gastrointestinal wall changes. Gastrointestinal wall changes were most common in the duodenum and identified in 71% (n = 22) of affected dogs. Of dogs with gastrointestinal wall changes, 74.2% (n = 23) had wall thickening, 61.3% (n = 19) had abnormal wall layering, and 35.5% (n = 11) had wall corrugation. In the multivariable model, only heart rate remained an independent predictor of ultrasonographic gastrointestinal wall changes. Conclusions and Clinical Importance: Ultrasonographic gastrointestinal wall changes in this population of dogs with AP were common. Increased heart rate was the only independent predictor of gastrointestinal wall changes, which might imply more severe disease. Additional studies are required to elucidate whether ultrasonographic gastrointestinal wall changes reflect disease severity in AP. ... In conclusion, ultrasonographic gastrointestinal wall changes were relatively common in this population of dogs with AP and were observed in approximately half of cases. Heart rate was the only clinical or clinicopathological variable independently associated with the presence of gastrointestinal wall changes. However, because of various possible contributing etiologies of tachycardia in this subset of dogs with AP, this finding is considered unlikely to be clinically useful in indicating whether GI wall changes are likely to be present. Our results however may aid clinicians in interpreting ultrasonographic gastrointestinal wall abnormalities in dogs with AP.
New insights into the etiology, risk factors, and pathogenesis of pancreatitis in dogs: potential impacts on clinical practice. Harry Cridge, Sue Yee Lim, Hana Algül, Jörg M. Steiner. J. Vet. Intern. Med. May 2022; doi: 10.1111/jvim.16437. Quote: While most cases of pancreatitis in dogs are thought to be idiopathic, potential risk factors are identified. In this article we provide a state-of-the-art overview of suspected risk factors for pancreatitis in dogs, allowing for improved awareness and detection of potential dog-specific risk factors, which might guide the development of disease prevention strategies. Additionally, we review important advances in our understanding of the pathophysiology of pancreatitis and potential areas for therapeutic manipulation based thereof. The outcome of pathophysiologic mechanisms and the development of clinical disease is dependent on the balance between stressors and protective mechanisms, which can be evaluated using the critical threshold theory.
Endocrine-Disrupting Chemicals and Their Effects in Pet Dogs and Cats: An Overview. Paola Pocar, Valeria Grieco, Lucia Aidos, Vitaliano Borromeo. Animals. January 2023; doi: 10.3390/ani13030378. Quote: Over the past few decades, several pollutants classified as environmental endocrine-disrupting chemicals (EDCs) have become a matter of significant public health concern. Companion animals play a major role in human society, and pet ownership is substantially increasing worldwide. These intimate human–pet relationships imply sharing much of the same environment, thus including exposure to similar levels of EDCs in daily routine. Here, we review the current knowledge on the sources and routes of exposure to EDCs in domestic indoor and outdoor environments and discuss whether endocrine disruption is a health concern in pets. We summarize the phenomenon of endocrine disruption, providing examples of EDCs with a known impact on dog and cat health. Then, we propose an overview of the literature on the adverse effects of EDCs in domestic pets, with a special focus on the health of reproductive and thyroid systems. Finally, we explore the potential role of companion animals as unintentional sentinels of environmental exposure to EDCs and the implications for public health risk assessment in a “shared risk” scenario. Overall, this review supports the need for an integrated approach considering humans, animals, and the environment as a whole for a comprehensive assessment of the impact of EDCs on human and animal health.
Pancreatitis, panniculitis, and polyarthritis syndrome in a dog with hyalinizing pancreatic adenocarcinoma. Abby Hagelskamp, Amelia G. White, Jeremy Gallman, Cierra Starbird, Rachel L. A. L. T. Neto. J. Vet. Diagnostic Investigation. September 2024; doi: 10.1177/10406387241267870. Quote: A 10-y-old spayed female Cavalier King Charles Spaniel dog was presented to the Veterinary Teaching Hospital because of recurrent chronic abscesses on the distal pelvic limbs, fever, lethargy, lameness of unknown etiology, and chronic pancreatitis. Sterile nodular panniculitis was diagnosed after an extensive workup, and the dog initially responded to immunosuppressive therapy, but relapse and spread of cutaneous lesions and acute lameness occurred after 11 mo, and euthanasia was elected. Postmortem examination confirmed hyalinizing pancreatic adenocarcinoma with pancreatitis, panniculitis, polyarthritis (PPP), and osteomyelitis. Histopathology and bacterial and fungal cultures were supportive of a sterile process, specifically the PPP syndrome, which is a rare, potentially life-threatening, systemic manifestation of pancreatic disease in both people and animals. To our knowledge, a clinicopathologic description of a hyalinizing pancreatic adenocarcinoma associated with this rare syndrome has not been reported previously in a dog.


CONNECT WITH US